The OASIS Item M1242, which assesses the frequency at which a patient’s pain interferes with activity, was retired on January 1, 2023. The new pain assessment items for OASIS E break down pain into three specific activities: pain affecting sleep, pain affecting rehabilitation activities, and pain affecting day-to-day activities. When documenting pain, clinicians must remember that pain is subjective and exists whenever the patient says it does. Clinicians ask patients to rate their pain on a scale of 0 to 10, with zero being no pain and 10 being the worst pain they have ever experienced.
| Characteristics | Values |
|---|---|
| Assessment | Frequency of Pain Interfering with patient’s activity or movement |
| Responses | 5 responses: no pain, rare, occasional, frequent, almost constant |
| Impact | Pain interferes with activity when a patient performs the activity less often than they want to, when they need assistance to complete the activity, or when the activity takes longer |
| Activities considered | Sleeping, watching TV, day-to-day activities, rehabilitation activities |
| Scoring | 0–10 scale, with 0 being no pain and 10 being the worst pain |
Explore related products
What You'll Learn

Pain interfering with sleep
The impact of pain on sleep is influenced by various factors, including the type and nature of the pain, physical health, mood, and sleeping position. For instance, individuals with hip, knee, or shoulder pain may need to avoid sleeping on their side, while those with pressure build-up in the lower back should consider their mattress and pillow to cushion pressure points. Additionally, the presence of anxiety, stress, or depression accompanying the pain can further exacerbate sleep problems.
To address pain interfering with sleep, it is important to consider both medical and non-medical interventions. Medical interventions may include chronic pain medications, while non-medical interventions can involve techniques such as guided imagery, distraction, and relaxation. Relaxation techniques, when practiced regularly, can help reduce nervous system activation and improve sleep. Other recommendations to improve sleep quality include maintaining a consistent wake-up time, avoiding exercise close to bedtime, and creating a favorable sleep environment with appropriate lighting and temperature.
In the context of the OASIS M1242 Pain Assessment, which evaluates the frequency of pain interfering with a patient's activity or movement, it is crucial to consider sleep as one of the activities. Inconsistencies between the M1242 score and a patient's pain diagnosis can have financial consequences and impact agency outcomes. Therefore, clinicians should carefully assess and document the impact of pain on a patient's sleep to determine appropriate modifications and improve overall quality of life.
The Constitution's Original Vision: A National Military?
You may want to see also

Pain impacting rehabilitation activities
Pain is a subjective experience, and it is influenced by various factors. It is essential to assess how pain impacts specific activities to determine the necessary modifications for improving patient outcomes and quality of life.
Rehabilitation activities are aimed at helping patients manage and reduce their pain. These activities can include physical modalities, behaviour modification, patient education, psychosocial rehabilitation, stress management, and vocational rehabilitation. For instance, physical activities like yoga, tai chi, swimming, and walking can effectively decrease pain and improve function. Additionally, exercise therapy, including aerobic exercises, flexibility exercises, and strength training, can be beneficial for pain management.
The OASIS M1242 assessment tool, which was retired on January 1, 2023, previously assessed the frequency at which a patient's pain interfered with their activities. It offered responses to capture how often pain interfered with a patient's ability to perform an activity, the need for assistance, or the time taken to complete the activity. However, inconsistencies could arise, such as patients reporting constant pain but also stating that it did not interfere with sleep.
To address these inconsistencies, the new OASIS E assessment breaks down pain evaluation into three specific activities: J0510, J0520, and J0530. Clinicians must document the frequency of pain, whether it is rare, occasional, frequent, or constant, and its impact on daily activities. This detailed assessment helps determine the necessary interventions to improve patient outcomes.
Rehabilitation teams typically consist of various healthcare professionals, including nurses, physicians, physiotherapists, psychologists, occupational therapists, and social workers. A successful rehabilitation process often includes the active participation of the patient and their family, with mutually agreed-upon goals focused on improving physical and psychological well-being, mobility, self-care, and social adjustment.
Understanding Oklahoma's Bill Revocation Process
You may want to see also

Pain affecting day-to-day activities
Pain is a highly subjective experience, and what one person considers severe may be different for another. As such, clinicians must remember that pain is whatever the patient says it is and exists whenever they say it does. With this in mind, the OASIS Item M1242, which assessed the frequency at which a patient's pain interfered with their activities, was retired on January 1, 2023. This was replaced by a more comprehensive assessment, OASIS-E, which breaks down pain into three specific activities: pain affecting sleep, rehabilitation activities, and day-to-day activities.
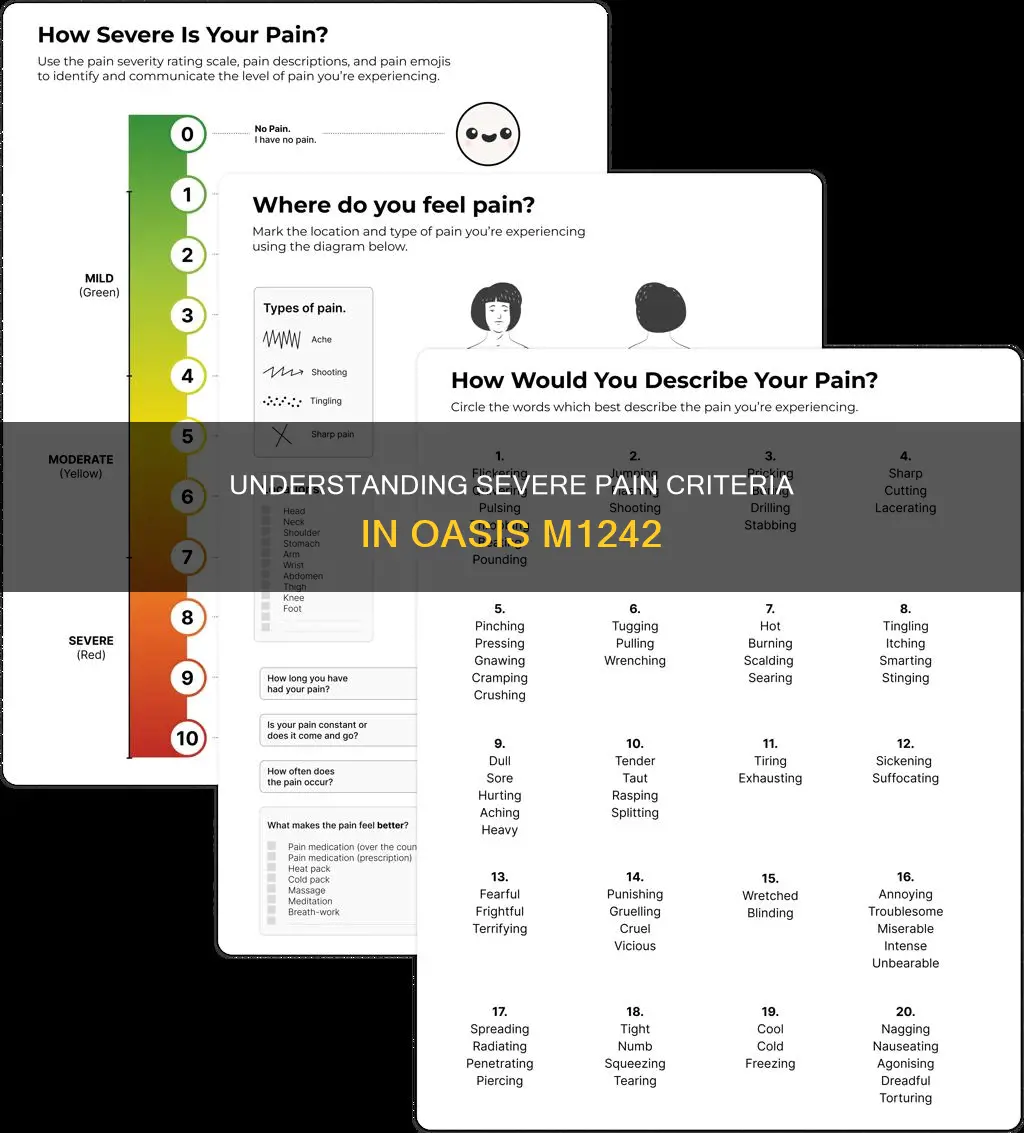
When documenting pain, clinicians can ask a series of questions to help evaluate a patient's response to treatment and develop interventions for a patient-specific plan of care. These questions include: What were you doing when the pain started? What caused it? What makes it better or worse? What relieves it? What aggravates it? What does it feel like? Where is the pain located? Does it feel like it moves around? How severe is the pain on a scale of 0 to 10, with zero being no pain and 10 being the worst pain imaginable?
In the context of day-to-day activities, pain can significantly impact a person's ability to perform basic tasks and maintain their independence. For example, a person with chronic back pain may find it challenging to walk, stand, or sit for extended periods, limiting their ability to perform daily activities such as grocery shopping or household chores. Similarly, a person with arthritis may experience severe pain when trying to open jars, lift objects, or write, affecting their ability to prepare meals or complete simple tasks.
The impact of pain on day-to-day activities can also vary depending on the time of day, the patient's energy levels, and the presence of any aggravating or relieving factors. For instance, a person with fibromyalgia may find that their pain worsens with physical activity, leading them to avoid exercise or limit their movements to manage their pain. However, this activity avoidance does not mean the absence of pain, as per OASIS guidance. Instead, it highlights the need for comprehensive pain management strategies, including medical interventions and non-medical techniques such as guided imagery, distraction, and relaxation.
Overall, when assessing pain's impact on day-to-day activities, clinicians should consider all aspects of a patient's life, including sleep and leisure activities, to develop effective interventions that improve patient outcomes and quality of life. By targeting specific activities affected by pain, clinicians can better determine the necessary modifications, such as recommending assistive devices or pain management techniques, to enhance the patient's functionality and overall well-being.
Who Has a Hard Copy of Oregon's Constitution?
You may want to see also
Explore related products
$167.14 $230

Pain intensity and location
When assessing pain intensity, clinicians ask patients to rate their pain on a scale from 0 to 10, with zero representing no pain and 10 being the worst pain imaginable. This subjective evaluation helps determine the severity of the patient's pain experience.
The location of the pain is also essential for accurate assessment and treatment planning. Clinicians inquire about the specific body areas where the patient experiences pain and whether it feels like it travels or moves around. This information helps identify any underlying conditions or issues that may be causing the pain.
It is important to note that pain is subjective, and its intensity can vary depending on various factors. Clinicians must document the patient's description of their pain, including qualities such as sharp, dull, stabbing, burning, throbbing, nauseating, or shooting pain. Additionally, understanding the factors that aggravate or relieve the pain, such as movement, resting, or medication, is crucial for developing an effective pain management plan.
In the context of OASIS M1242, pain intensity and location are no longer assessed in isolation but are considered in relation to specific activities. For example, when assessing the impact of pain on sleep, clinicians ask patients how much of the time pain has interfered with their sleep over the past five days. This information is then coded accordingly, with responses ranging from "no pain" to "almost constantly." By considering pain in relation to specific activities, clinicians can better evaluate the need for interventions and modifications to improve patient outcomes and quality of life.
Constitutions Inspired by the US: A Global Influence
You may want to see also

Pain relief methods
The experience of pain is subjective and influenced by a person's emotional well-being. It is important to use a variety of strategies to help reduce pain and not rely solely on medicines.
Medication
Paracetamol is often recommended as the first medicine to relieve short-term pain. Aspirin is also used for short-term relief from fever and mild-to-moderate pain. Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, relieve pain and reduce inflammation. Opioid medicines, such as codeine, morphine, and oxycodone, are reserved for severe or cancer pain. Local anaesthetics (drops, sprays, creams, or injections) are used when nerves can be easily reached. Some antidepressants and anti-epilepsy medicines are used for nerve pain.
Physical Therapies
These include exercise, physical therapy, and occupational therapy. Simple everyday activities like walking, swimming, gardening, and dancing can ease pain by blocking pain signals to the brain and stretching stiff and tense muscles, ligaments, and joints. It is important to increase activity gradually to avoid causing damage or harm. Physical therapists guide patients through exercises designed to preserve or improve strength and mobility. Occupational therapists help patients perform daily activities without aggravating their pain.
Complementary Therapies
These include acupuncture and massage.
Mind-Body Techniques
These techniques include meditation, mindfulness, and breathing exercises, which help restore a sense of control over the body and reduce the "fight or flight" response, which can worsen chronic muscle tension and pain. Yoga and tai chi are two practices that incorporate breath control, meditation, and gentle movements to stretch and strengthen muscles.
Psychological Therapies
Psychological therapies, such as cognitive behavioural therapy, can help patients cope with their emotions related to pain. Hypnotherapy and talking therapies can also be useful.
The Vast Emptiness Within Atoms
You may want to see also
Frequently asked questions
M1242 of the OASIS assessment refers to the frequency of pain interfering with a patient's activity or movement.
Severe pain is constituted by a score of 8-10 on a scale of 0 to 10, with zero being no pain and 10 being the worst pain the patient has ever experienced.
M1242 offers five different responses to capture how frequently a patient's pain is interfering with their activities: 0 (no pain), 1 (pain rarely interferes with activity), 2 (occasionally), 3 (frequently), and 4 (almost constantly).
All activities, including sleeping, watching TV, and other day-to-day activities, should be considered when completing M1242, not just ADLs.
According to the OASIS-C2 Guidance Manual, a maximum of three case-mix points are available if the answer to M1242 is a "3" or a "4," depending on episode timing and therapy utilization.