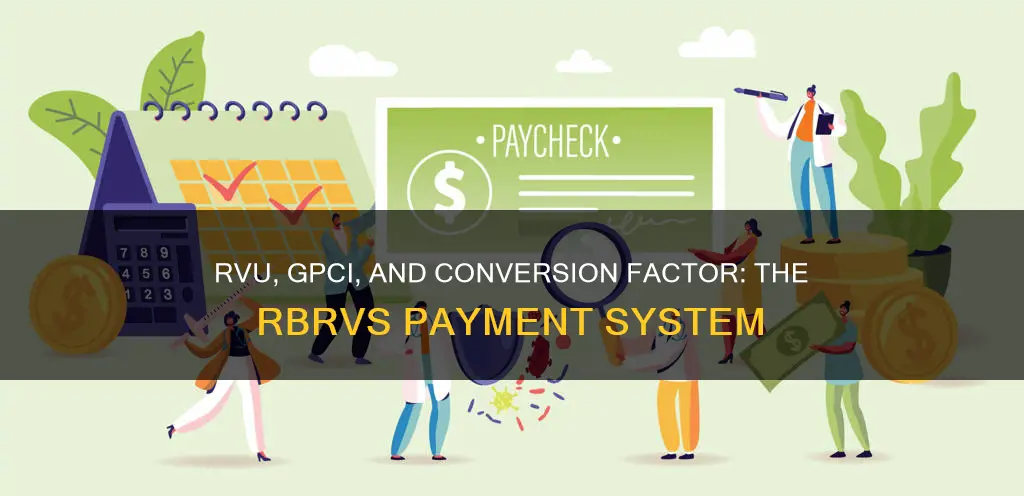
The Resource-Based Relative Value Scale (RBRVS) is a system used in the United States to determine reimbursement rates for medical services provided by healthcare professionals. RBRVS payment systems are based on three components: physician work, practice expense, and malpractice expense. The RBRVS system was established in 1992 and is used by the Centers for Medicare and Medicaid Services (CMS) and most other payers. It is designed to improve and stabilize the payment system and provide physicians with an avenue to continuously improve it. Payments are calculated by multiplying the combined costs of a service by a conversion factor, which is a monetary amount determined by CMS, and adjusting for geographical differences in resource costs.
| Characteristics | Values |
|---|---|
| Number of Components | 3 |
| Component 1 | Physician work |
| Component 2 | Practice expense |
| Component 3 | Malpractice expense/insurance/liability insurance |
| Calculation | Relative value units (RVUs) of each component x Conversion factor (CF) |
| Conversion Factor | Monetary amount determined by CMS, updated annually |
| Relative Value Units | Determined by Specialty Society Relative Value Scale Update Committee (RUC) |
| Relative Value Weights | Physician work (52-54%), Practice expense (41-44%), Malpractice expense (4-5%) |
| Additional Factors | Geographic location, Resource costs, Physician specialty |
Explore related products
What You'll Learn
- Physician work, practice expense, and malpractice expense/insurance are the three components
- RBRVS is used to determine reimbursement rates for medical services
- RBRVS is a more standardised and equitable approach to reimbursement
- RBRVS is based on the principle that payments should vary with resource costs
- RBRVS is used by CMS and most other payers

Physician work, practice expense, and malpractice expense/insurance are the three components
The Resource-Based Relative Value Scale (RBRVS) is a system used in the United States to determine the reimbursement rates for medical services provided by healthcare professionals. RBRVS is based on the principle that payments for physician services should vary according to the resource costs for providing those services. The RBRVS payment system is constituted by three components: physician work, practice expense, and malpractice expense/insurance.
The RBRVS assigns a relative value to each medical service based on these three components. The relative value is calculated by considering factors such as time, effort, skill, and resources required to perform the service. Physician work, which includes the physician's time, mental effort, technical skill, judgment, stress, and the amortization of the physician's education, typically accounts for the largest proportion of the relative value, with an average weight of 52-55%. Practice expense, which includes direct expenses related to supplies and non-physician labor, as well as the pro-rata cost of equipment and indirect expenses, accounts for an average of 41-45% of the total relative value. The malpractice expense component accounts for the remaining 4-5% of the relative value and reflects the cost of professional liability insurance incurred by healthcare providers. It is calculated based on historical malpractice insurance data and the risk associated with the specific medical service.
Once the relative value for each service is determined, it is multiplied by a conversion factor, also known as a fixed monetary amount or CF, to obtain the reimbursement rate. The CF is set annually by Congress when they work on the Medicare budget and varies between $30 and $50. This conversion factor is used to convert the relative values assigned to each procedure code into monetary values. The RBRVS system also includes a geographic adjustment factor (GAF) or Geographic Practice Cost Index (GPCI) to account for locality cost differences across the country.
The RBRVS was established in 1992 and is widely used by public and private payers, including Medicare and many third-party payers, to establish payment rates for physicians, nurse practitioners, and other healthcare providers. It provides a more standardized and equitable approach to reimbursement, ensuring fair compensation for healthcare providers based on the resources required to deliver quality care.
Amendments Removed: A Constitutional Evolution
You may want to see also

RBRVS is used to determine reimbursement rates for medical services
The Resource-Based Relative Value Scale (RBRVS) is a system used to determine reimbursement rates for medical services. RBRVS is used by the Centers for Medicare and Medicaid Services (CMS) and most other payers. RBRVS was first introduced by Medicare in 1992 to try to reduce Medicare's expenditures for physician services and to decrease the variation in physician payments across different procedures, specialties, and geographic locations.
The RBRVS payment system is based on the principle that payments for physician services should vary with the resource costs for providing those services. RBRVS is intended to improve and stabilize the payment system while providing physicians with an avenue to continuously improve it. RBRVS assigns procedures performed by a physician or other medical provider a relative value that is adjusted by geographic region. This value is then multiplied by a fixed conversion factor, which changes annually, to determine the amount of payment.
The RBRVS for each CPT code is determined using three separate factors: physician work, practice expense, and malpractice expense. The average relative weights of these are: physician work (52%), practice expense (44%), and malpractice expense (4%). The RBRVS does not include adjustments for outcomes, quality of service, severity, or demand.
The calculation of the fee includes a geographic adjustment. Payments are calculated by multiplying the combined costs of a service by a conversion factor (a monetary amount determined by CMS) and adjusting for geographical differences in resource costs.
Citing the Constitution Act 1982: APA Style Guide
You may want to see also

RBRVS is a more standardised and equitable approach to reimbursement
The Resource-Based Relative Value Scale (RBRVS) is a system used to determine reimbursement rates for medical services provided by healthcare professionals. RBRVS is based on the principle that payments for physician services should vary according to the resource costs of providing those services. It is intended to improve and stabilise the payment system while providing physicians with an avenue to continuously improve it. RBRVS is a more standardised and equitable approach to reimbursement for several reasons.
Firstly, RBRVS is designed to ensure fair compensation for healthcare providers based on the resources required to deliver quality care. It considers factors such as physician work, practice expenses, and malpractice expenses to assign a relative value to each service. This relative value is then multiplied by a conversion factor, or monetary amount, to calculate the reimbursement rate. By taking into account the different factors involved in providing medical services, RBRVS aims to determine appropriate reimbursement rates. For example, a primary care physician providing a routine office visit may be assigned a lower relative value than a specialist performing a complex surgical procedure that requires significant physician work and extensive practice expenses.
Secondly, RBRVS provides a standardised framework for reimbursement by incorporating three main components: physician work, practice expense, and malpractice expense or professional liability insurance. These components are further broken down into various factors such as time, effort, skill, and resources required to perform the service. By considering these standardised components, RBRVS aims to ensure that reimbursement rates are calculated consistently across different medical services and providers.
Thirdly, RBRVS includes a geographic adjustment factor, recognising that the value of a procedure can vary depending on the geographic region in which it is performed. This adjustment factor, known as the Geographic Practice Cost Index (GPCI), is applied to account for locality cost differences for work, practice expense, and liability coverage across the country. This ensures that reimbursement rates are equitable and take into consideration geographic variations in resource costs.
Finally, RBRVS is continually updated and improved through initiatives by governmental and specialty society relative value scale update committees (RUC). These committees meet regularly to set new values, determine Relative Value Units (RVUs), and revalue existing codes to reflect changing circumstances and needs in the healthcare industry. This ongoing review process helps to ensure that the RBRVS system remains relevant, equitable, and responsive to the complex landscape of healthcare revenue cycle management.
Exploring the Core Differences: Constitution vs Declaration of Independence
You may want to see also
Explore related products

RBRVS is based on the principle that payments should vary with resource costs
The Resource-Based Relative Value Scale (RBRVS) is a system used to determine how much medical providers should be paid. RBRVS is based on the principle that payments should vary with resource costs, and it is used by the Centers for Medicare and Medicaid Services (CMS) and most other payers. RBRVS assigns procedures performed by a physician or other medical provider a relative value, which is adjusted by geographic region. This value is then multiplied by a fixed conversion factor, which changes annually, to determine the amount of payment.
The RBRVS system has been criticized for paying based on effort rather than effect, which may lead to overuse of complicated procedures without consideration for outcomes. According to this critique, RBRVS misaligns incentives as there is no financial incentive to help the patient or minimize costs. Rather, payment is based on the difficulty of the service, and thus a profit-maximizing physician is incentivized to provide maximally complicated services, with no consideration for effectiveness.
However, despite the criticisms, the RBRVS proved to be a giant leap toward supporting a fair and equitable basis for physician compensation. The RBRVS calculates payment based on the costs of providing medical procedures and services. This is in contrast to the previous system, where physicians set charge rates for the medical care they provided to patients, which led to considerable variance in physician compensation.
The RBRVS determines prices based on three separate factors: physician work, practice expense, and malpractice expense. The average relative weights of these are: physician work (52-54%), practice expense (41-45%), and malpractice expense (4-5%). The RBRVS for each CPT code is determined using these three separate factors. The CPT committee issues new codes twice each year.
Constitutional Provisions: Different Interpretations Than Statues?
You may want to see also

RBRVS is used by CMS and most other payers
The Resource-Based Relative Value Scale (RBRVS) is a system used in the United States to calculate the amount of money that insurers will pay healthcare providers for their services. RBRVS is used by the Centers for Medicare and Medicaid Services (CMS) and most other payers.
RBRVS was established in 1992 when Medicare significantly changed the way it pays for physician services. Instead of basing payments on charges, the federal government established a standardized RBRVS-based physician payment schedule. RBRVS is based on the principle that payments for physician services should vary with the resource costs for providing those services. The RBRVS for each CPT code is determined using three separate factors: physician work, practice expense, and malpractice expense.
The RBRVS is used by CMS to calculate fees for each service and procedure based on a single measure: the RVUs. The RVUs are the basic components that are plugged into the RBRVS formula. The RBRVS formula adjusts for geographic location and multiplies by a conversion factor set by the CMS each year. The conversion factor is a monetary amount determined by CMS.
The RBRVS is also used by many non-Medicare payers, including private health plans. The RBRVS determines prices based on the three separate factors mentioned earlier: physician work (52-54%), practice expense (44%-41%), and malpractice expense (4-5%). The RBRVS is maintained by CMS, and the AMA/Specialty Society RVS Update Committee (RUC) provides relative value recommendations to CMS annually.
Electoral Systems: Which Country Reigns Supreme?
You may want to see also
Frequently asked questions
The RBRVS payment system is based on three components: physician work, practice expense, and malpractice expense (also known as professional liability insurance).
The Resource-Based Relative Value Scale (RBRVS) is a system used to determine reimbursement rates for medical services in the United States. It aims to provide a standardised and equitable approach to reimbursement, ensuring fair compensation for healthcare providers based on the resources required to deliver quality care.
The RBRVS assigns a relative value to each medical service based on the three components mentioned above. This relative value is then multiplied by a conversion factor, which is a monetary amount determined by the Centers for Medicare and Medicaid Services (CMS), to calculate the reimbursement rate. The RBRVS also includes a geographic adjustment factor to account for differences in locality costs.