The CDC classification system for HIV infection is the medical classification system used by the United States Centers for Disease Control and Prevention (CDC) to classify HIV disease and infection. The system is used to allow the government to handle epidemic statistics and define who receives US government assistance. The classification system reflects the stage of the disease, establishes mutually exclusive classification categories, and balances simplicity and medical accuracy in the classification process. The clinical manifestations of patients in this group may be designated by assignment to one or more subgroups (A-E). The CD4 count provides another marker for characterizing the clinical stages. AIDS has been defined as the laboratory diagnosis of HIV infection plus either an opportunistic infection or a CD4 count of below 200/μL.
Explore related products
What You'll Learn

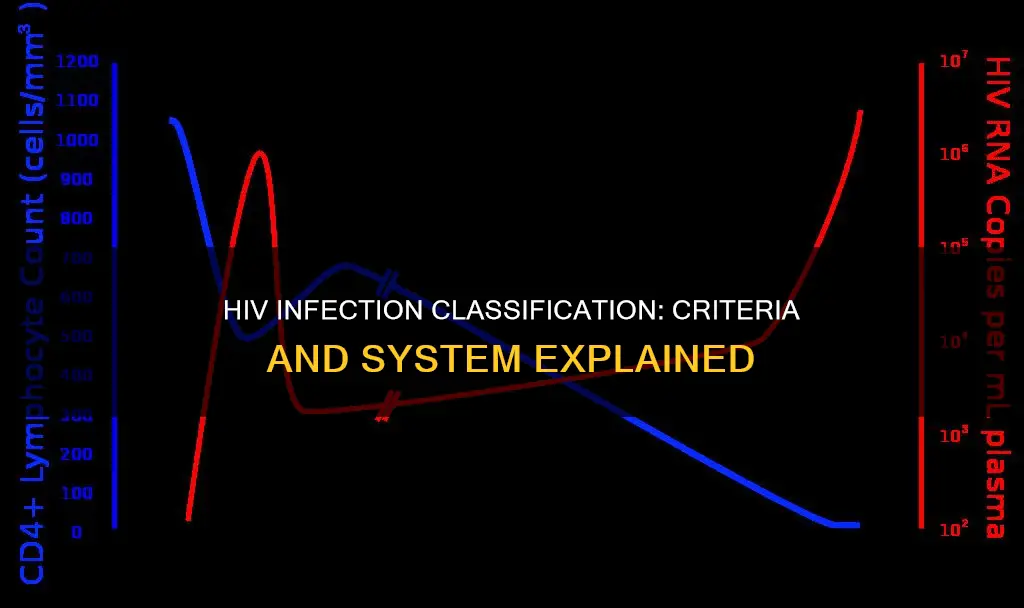
CD4+ T-cell count
CD4 cells, also known as CD4+ T lymphocytes or "helper T cells", are a type of white blood cell that circulates throughout the body in the blood. They play a critical role in the immune system by triggering an immune response to destroy viruses, bacteria, and other germs that may cause illness.
HIV (human immunodeficiency virus) attacks and destroys CD4 cells. Without treatment, HIV may destroy so many CD4 cells that the body will struggle to fight off infections. A CD4 count is a blood test that measures the number of CD4 cells in a sample of blood and is used to check the health of the immune system in people infected with HIV. The CD4 count of a person who does not have HIV can be anywhere between 500 and 1500.
The CD4 count is used to evaluate the progression of HIV and should be measured at the time of initial diagnosis. The test is also an indicator of treatment failure. If CD4 levels drop below 200 cells/mm3, this is an indication of an AIDS diagnosis. When the CD4 count falls below 200, there is a high risk of opportunistic infections and serious illnesses.
For people living with HIV, CD4 counts are monitored regularly, especially during the first months of treatment. This is because CD4 counts help to assess the risk of opportunistic infections and certain cancers. If a patient's risk increases, their doctor may give them treatment to help prevent infections. CD4 counts are also used together with an HIV viral load test to see if HIV medicines are working.
Trump's Constitutional Challenge: Congress Responds
You may want to see also

Clinical conditions
The CDC's classification system for HIV infection considers a range of clinical manifestations. Group III includes patients with persistent generalised lymphadenopathy, a condition characterised by enlarged lymph nodes. Group IV encompasses patients presenting with clinical symptoms and signs of HTLV-III/LAV infection, beyond lymphadenopathy. This group is further subdivided into categories, including constitutional disease, neurologic disease, secondary infectious diseases, secondary cancers, and other conditions attributed to HTLV-III/LAV infection.
Within Group IV, Subgroup A comprises constitutional disease, marked by symptoms such as persistent fever for more than a month, involuntary weight loss exceeding 10% of baseline, and persistent diarrhea for over a month. These symptoms must occur in the absence of other explanatory illnesses or conditions. Subgroup B addresses neurologic manifestations, while Subgroup C focuses on secondary infectious diseases that arise alongside HIV infection.
Subgroup D pertains to secondary cancers that develop in the context of HIV infection. This subgroup includes cancers such as Hodgkin's disease, non-Hodgkin's lymphoma, lymphocytic leukaemia, multiple myeloma, and cancers affecting lymphoreticular or histiocytic tissues. Additionally, Subgroup E captures a range of other clinical findings or diseases attributed to HTLV-III/LAV infection, including chronic lymphoid interstitial pneumonitis.
The CDC's classification system has been periodically updated to reflect new knowledge about HIV and AIDS. For instance, in 1993, the CDC expanded the AIDS surveillance case definition to encompass all HIV-infected individuals with specific CD4+ T-lymphocyte counts or percentages, adding pulmonary tuberculosis, recurrent pneumonia, and invasive cervical cancer to the list of clinical conditions.
Furthermore, the classification system acknowledges differences in clinical presentations between adults and children. For instance, multiple or recurrent serious bacterial infections and lymphoid interstitial pneumonia are considered indicative of AIDS in children but not adults. The system also recognises the challenges in diagnosing HIV infection in infants born to infected mothers due to the presence of maternal anti-HIV IgG antibodies.
Vascular System: Plants' Intricate Water Transport Network
You may want to see also

Pediatric HIV classification
The CDC classification system for HIV infection is the medical classification system used by the United States Centers for Disease Control and Prevention (CDC) to classify HIV disease and infection. In 1994, a revised classification system for HIV infection in children replaced the paediatric HIV classification system that was published in 1987. This was due to additional knowledge of the progression of HIV disease among children.
The 1994 classification system defines a child as an individual of less than 13 years of age. It also outlines that standard anti-HIV IgG antibody tests cannot reliably indicate a child's infection status before 18 months of age, so viral antigen tests are used.
The system categorises HIV-infected children into mutually exclusive categories according to three parameters:
- The stage of the child's disease
- The presence or absence of symptoms considered to be the result of HIV infection
- The CD4+ T-cell count or percentage
The CD4+ T-cell count takes precedence over the CD4+ percentage, and the percentage is considered only when the count is missing. The categories are designed to be simple yet medically accurate and include revised paediatric definitions for two acquired immunodeficiency syndrome-defining conditions.
When an infant is born to an HIV-infected mother, the diagnosis of an HIV infection is complicated by the presence of maternal anti-HIV IgG antibodies, which cross the placenta to the fetus. Therefore, virtually all children born to HIV-infected mothers are HIV-antibody positive at birth, although only 15%-30% are actually infected.
How Federal Judges Interpret the US Constitution
You may want to see also
Explore related products

HIV antibody presence
HIV antibody tests are a crucial tool in the diagnosis of HIV infection and the subsequent initiation of life-saving treatment. These tests detect the presence of HIV antibodies in the blood or oral fluid, which are disease-fighting proteins produced by the body in response to HIV infection. The timing of the test is critical as it takes time for the body to generate antibodies after exposure to HIV.
The presence of HIV antibodies in an individual's system can be indicative of an active infection. However, it is important to understand the window period, which is the time between potential HIV exposure and the point at which a test can accurately detect the infection. This window period varies for different tests, including antibody tests, antigen/antibody tests, and nucleic acid tests (NATs). NATs, which detect the virus itself in the blood, can usually identify HIV as soon as 10 to 33 days after infection. In contrast, antibody tests typically take longer to detect HIV as they rely on the body's production of antibodies, which may take 3 to 12 weeks after infection.
The antibody response to HIV infection is complex and involves various antibody isotypes, such as IgM, IgG, IgA, and IgE. These antibodies target the proteins encoded by HIV genes, and their specificities can provide insights into the detrimental effects of HIV on B cell and T cell responses. Unfortunately, the initial antibody response during acute HIV-1 infection is often ineffective in controlling virus replication, allowing the establishment of HIV latency.
In the context of pregnancy and childbirth, the presence of maternal anti-HIV IgG antibody can complicate the diagnosis of HIV infection in infants born to HIV-infected mothers. These infants are typically HIV-antibody positive at birth due to the transfer of maternal antibodies through the placenta. However, only 15%-30% of these infants are actually infected. Therefore, alternative testing methods, such as viral antigen tests, are necessary to accurately determine the infection status of infants before 18 months of age.
The classification systems for HIV infection, such as the CDC classification system, play a crucial role in defining access to government assistance and managing epidemic statistics. The presence or absence of HIV antibodies is a critical component of these classification systems, helping to determine the stage of disease progression and guiding the development of exclusive classification categories. By combining antibody testing with clinical presentations and CD4+ T-cell counts, healthcare providers can make accurate diagnoses and provide appropriate treatment and support.
Core Values of the Confederate Constitution
You may want to see also

Opportunistic infections
OIs are caused by a variety of germs (viruses, bacteria, fungi, and parasites) and can be spread through the air, body fluids, contaminated food or water, and sexual contact. Some of the most common OIs in people with HIV include:
- Herpes simplex virus 1 (HSV-1) infection—a viral infection that can cause eye inflammation, mouth and throat disease, genital herpes, and brain infections.
- Salmonella infection—a bacterial intestinal infection.
- Candidiasis (thrush)—a fungal infection of the mouth, bronchi, trachea, lungs, esophagus, or vagina.
- Toxoplasmosis—a parasitic brain infection.
- Pneumocystis pneumonia (PCP)—a lung infection caused by a fungus.
- Tuberculosis—a bacterial lung infection that can also affect the kidneys, brain, skin, lymph nodes, and eyes.
OIs are less common now than they were in the early days of HIV and AIDS due to the development of antiretroviral therapy (ART), which reduces the amount of HIV in a person's body and strengthens their immune system. However, patients who present in the late stages of HIV or are unable to maintain viral suppression remain at high risk for OIs.
To reduce their risk of getting an OI, people with HIV can take HIV medicines as prescribed, use condoms during sexual activity, avoid sharing drug injection equipment, and practice good hygiene, especially after contact with human or animal feces.
Understanding the WHO's Definition of Health
You may want to see also
Frequently asked questions
The CDC classification system for HIV infection is the medical classification system used by the United States Centers for Disease Control and Prevention (CDC) to classify HIV disease and infection.
According to the US CDC, a person has AIDS if they are infected with HIV and have a CD4+ T-cell count below 200 cells per milliliter of blood or develop certain illnesses, sometimes called opportunistic infections.
The CDC classification system for HIV infection has a separate set of criteria for children, as standard anti-HIV IgG antibody tests cannot be used to reliably indicate a child's infection status before 18 months of age. HIV-infected children are classified into mutually exclusive categories according to three parameters that reflect the stage of the child's disease.
The Walter Reed staging system of HIV infection classifies patients based on CD4 counts, skin-test responsiveness, lymphadenopathy, oral candidiasis, and opportunistic infections. The World Health Organization (WHO) has also developed a case definition for AIDS that describes the clinical conditions arising from immune deficiency.
The CDC classification system for HIV infection has been updated since its inception in 1986. For example, in 1993, the CDC added pulmonary tuberculosis, recurrent pneumonia, and invasive cervical cancer to the list of clinical conditions. In 1994, a revised classification system for HIV infection in children was developed, replacing the pediatric HIV classification system from 1987.