Medicare's 8-Minute Rule, also known as the Rule of Eights, is a billing practice that dictates that healthcare providers must offer at least eight minutes of direct, one-on-one patient care to bill for one unit of a timed service. This rule was introduced to ensure accurate and fair reimbursement for outpatient services, such as physical, occupational, and speech therapy, and it applies to all federal payers and some commercial payers. The rule can be tricky to navigate, and incorrect billing can result in penalties and missed revenue.
| Characteristics | Values |
|---|---|
| Minimum time for a single "billable unit" | 8 minutes |
| Maximum time for a single "billable unit" | 22 minutes |
| Minimum time for two "billable units" | 23 minutes |
| Time for one "billable unit" in minutes | 15 minutes |
| Rule | 8-minute rule |
| Other names for the rule | Rule of Eights, Medicare Rule of 8's, 8 min rule |
| Applicable to | Physical therapy, occupational therapy, speech therapy, outpatient therapy services, inpatient acute settings |
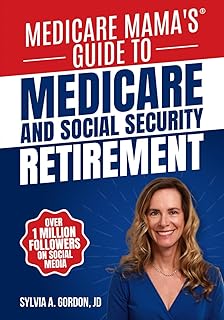
Explore related products
What You'll Learn

The 8-minute rule
Medicare's 8-minute rule, introduced in 1999 and fully adopted in 2000, dictates that healthcare providers must deliver at least eight minutes of direct, one-on-one, face-to-face patient care to bill for one unit of a timed service. This rule ensures accurate and fair reimbursement for outpatient services, such as physical, occupational, and speech therapy. It is important for beneficiaries to understand this rule to know how their Medicare coverage is charged for these services.
To calculate the number of billable units, the total minutes of skilled, one-on-one therapy are added up and then divided by 15. If 8 or more minutes remain, an additional unit can be billed; if 7 or fewer minutes remain, an extra unit cannot be billed. For example, if a therapist provides 33 minutes of therapeutic exercises, this would be divided by 15, resulting in 2 units. Since the remainder of 3 is less than 8, no additional unit can be added.
There are other Medicare rules and modifiers that apply to billing under the 8-minute rule. For example, the CQ or CO modifier indicates services performed by a physical or occupational therapy assistant, and the GA modifier shows that the provider has an Advanced Beneficiary Notice on file for noncoverage of a service.
Democracy's Principles: The US Constitution's Foundation
You may want to see also

Calculating billable units
Medicare introduced the 8-minute rule in 1999 and fully adopted it in 2000. The 8-minute rule is a method of determining how many billable units can be charged for time-based services during a single patient visit. The rule states that a healthcare provider must provide at least eight minutes of direct, face-to-face patient care to bill for one unit of a timed service. Anything less than that does not qualify as billable time. The rule helps ensure accurate and fair reimbursement for outpatient services, such as physical, occupational, and speech therapy.
To calculate the appropriate number of units for billing, follow these steps:
- Add all the time spent on timed services to determine the total number of billable units: For example, a therapist spent 35 minutes doing therapeutic exercises (97110) and 15 minutes on manual therapy (97140). So the total time spent with the patient was 50 minutes.
- Separate each whole 15-minute unit by CPT code: For the above example, two units of 97761 would equal 30 minutes.
- Handle any remaining minutes that have not been converted into whole units: If 8 or more minutes are left over, the therapist can bill for one more unit. If 7 or fewer minutes remain, the therapist cannot bill an additional unit.
The 8-minute rule is a tricky business, and many find themselves unsure of the right path forward. Billing for the wrong number of units can result in penalties for upcoding. It is important to have technology that makes it easy to follow Medicare billing guidelines.
Franklin's Influence on the US Constitution
You may want to see also

Timed Common Procedure Terminology (CPT) codes
Timed CPT codes are used for billing Medicare for timed physical therapy services. CPT stands for Current Procedural Terminology, and these codes are used by doctors and healthcare professionals as a uniform language for coding medical services and procedures. CPT codes are also used for administrative management purposes such as claims processing and developing guidelines for medical care review.
The CPT code set is maintained by the American Medical Association (AMA) through the CPT Editorial Panel. The CPT code set describes medical, surgical, and diagnostic services and is designed to communicate uniform information about medical services and procedures among physicians, coders, patients, accreditation organizations, and payers for administrative, financial, and analytical purposes. There are three types of CPT codes: Category I, Category II, and Category III.
Category I CPT codes are used for reporting services or procedures performed by physicians and other healthcare providers, tests and drugs (including vaccines) required for the performance of a service or procedure. Category II codes are alphanumeric tracking codes used for reporting performance measures, reducing the necessity for chart review and medical records abstraction. They are reviewed by the Performance Measures Advisory Group (PMAG), an advisory body to the CPT Editorial Panel and the CPT/HCPAC Advisory Committee. Category III codes are temporary alphanumeric codes for new and developing technology, procedures, and services.
The Medicare 8-Minute Rule dictates that healthcare providers must provide at least eight minutes of direct, face-to-face patient care to bill for one unit of a timed service. Anything less than that does not qualify as billable time. To calculate the number of billable units, Medicare adds up the total minutes of skilled, one-on-one therapy and divides that total by 15. If 8 or more minutes are left over, the therapist can bill for one more unit; if 7 or fewer minutes remain, the therapist cannot bill an additional unit.
The Constitution's Power Division: A Guide
You may want to see also
Explore related products
$22.79 $35.99

Medicare billing for inpatient hospital care
The billing process for inpatient hospital care can vary depending on the specific services rendered and the patient's insurance coverage. For example, Medicare Part A covers inpatient hospital stays, but the number of covered days varies. The first 60 days incur no additional costs after meeting the Part A deductible, days 61-90 result in a daily charge, and days beyond 90 incur higher daily charges up to a maximum of 60 lifetime reserve days. After exhausting the lifetime reserve days, the patient becomes responsible for all costs.
Medicare also covers inpatient mental health care, but the number of covered days differs between freestanding psychiatric hospitals and Medicare-certified psychiatric units within acute care or critical access hospitals. Part B of Medicare generally covers 80% of the Medicare-approved amount for doctors' services received during a hospital stay. Additionally, Medicare has specific rules for billing timed services, known as the 8-Minute Rule, which applies to outpatient services like physical, occupational, and speech therapy.
The 8-Minute Rule dictates that healthcare providers must deliver at least eight minutes of direct, face-to-face patient care to bill for one unit of a timed service. Each 15-minute increment thereafter can be billed as an additional unit. This rule helps ensure fair reimbursement and prevents upcoding or overcharging. It is essential for therapists and billing professionals to understand this rule to avoid errors in billing and potential penalties.
To summarize, Medicare billing for inpatient hospital care is a complex process influenced by the patient's hospital status, the duration of their stay, the type of services provided, and the specific rules and coverage of the patient's Medicare plan. Hospitals are required to share their standard charges publicly to help patients make informed decisions about their care. However, patients may still incur out-of-pocket expenses for services not covered or fully reimbursed by Medicare.
The Constitution: Ratification and the States
You may want to see also

Therapy services
Medicare Part B helps pay for medically necessary outpatient physical therapy, which helps to restore or improve physical movement in the body after an injury, illness, or surgery. There is no limit on how much Medicare pays for medically necessary outpatient therapy services in a calendar year. After meeting the Part B deductible, the patient pays 20% of the Medicare-approved amount.
The 8-minute rule is also known as the Medicare Rule of 8's, and it is a crucial aspect of physical therapy billing and documentation. It directly influences the calculation of billable units and the documentation of time-based services. It is important for therapists to understand this rule to ensure accurate billing and compliance with Medicare's guidelines.
There are certain modifiers that might impact the claim's reimbursement. For instance, CQ or CO designates services performed in whole or in part by a physical or occupational therapy assistant. The GA modifier indicates that the provider has an Advanced Beneficiary Notice (ABN) on file for non-coverage of a service that Medicare does not consider medically necessary. The GO modifier shows that an OT has provided services, usually in an inpatient or outpatient therapy setting.
Drafting a Constitution: A Guide for Organizations
You may want to see also
Frequently asked questions
The 8-minute rule dictates that healthcare providers must provide at least 8 minutes of direct, face-to-face patient care to bill for one unit of a timed service.
The 8-minute rule applies to inpatient and outpatient therapy services, including physical therapy, occupational therapy, and speech therapy.
To calculate the number of billable units, you add up the total minutes of skilled, one-on-one therapy and divide that total by 15. If 8 or more minutes are left over, you can bill for one more unit. If 7 or fewer minutes remain, you cannot bill an additional unit.
The 8-minute rule is followed by all federal payers and some commercial payers. It applies to Medicare and other federally funded insurance providers like TRICARE and Medicaid.
Yes, the 8-minute rule does not apply to group therapy, complex cases, and service-based CPT codes. Some telehealth services may also be exempt, but this is determined on a case-by-case basis.