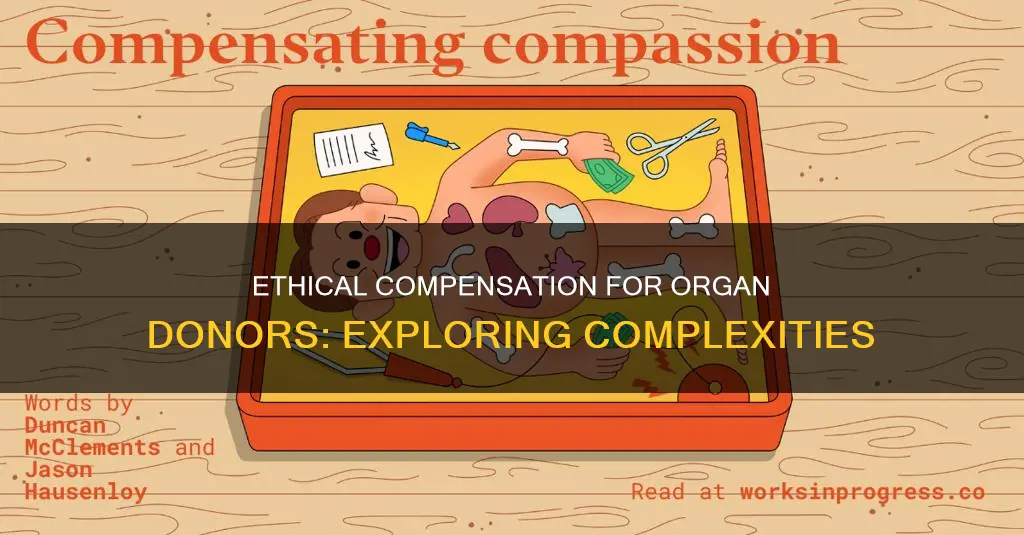
Organ donation is a life-saving medical procedure, but the demand for donor organs far exceeds the supply. To address this, some have proposed compensating donors for their donations. While this strategy has been implemented in several systems internationally, it is prohibited by law in many countries, including the United States, where the National Organ Transplant Act (NOTA) bans the transfer of human organs for valuable consideration. However, there is ongoing debate about the ethics and effectiveness of compensating organ donors, with some arguing that it could increase the availability of organs for transplant, while others raise concerns about exploitation and inequality.
| Characteristics | Values |
|---|---|
| Reimbursement of expenses | Travel, housing, lost wages incurred during evaluation, surgery and aftercare |
| Financial incentives | Cash payments, tax deductions, tax credits, tuition vouchers, 401(k) contributions, Medicare vouchers |
| Priority access | Priority access to organs for family members |
| Other incentives | N/A |
Explore related products
What You'll Learn

The ethics of compensating organ donors
The topic of compensating organ donors raises ethical questions and divides opinions. While some people argue that organ donors should be compensated, others believe that introducing financial incentives could exploit the poor and desperate and undermine the spirit of altruism.
In the United States, the National Organ Transplant Act (NOTA) prohibits the transfer of human organs "for valuable consideration". However, it allows for the removal of financial disincentives, such as reimbursing donors for travel, housing, and lost wages incurred during evaluation, surgery, and aftercare. Several proposals exist to compensate patients for living donations, including reimbursing costs incurred as part of the donation process.
Some countries, like Iran, India, and Pakistan, permit the compensated donation of organs. In Iran, the government regulates the program to ensure donors receive reasonable compensation. However, this practice raises ethical and legal concerns related to exploitation and inequality, especially when the donor is poor and the recipient is wealthy.
Proponents of compensating organ donors argue that it could help address the dire shortage of organs available for transplant. Dr. Sally Satel, for example, believes that "we have to reward people who are willing to give a kidney to a stranger as a way to motivate others to do the same". She suggests forms of compensation that wouldn't appeal to the poor and desperate, such as tax credits, tuition vouchers, or Medicare vouchers.
According to an NPR opinion poll, about 60% of Americans would support modest compensation for organ donation under specific circumstances. Support for compensation was higher among younger individuals and those with higher education levels.
As the debate around compensating organ donors continues, it is essential to carefully consider the potential benefits and risks of introducing financial incentives to ensure that any policy changes are ethical and in the best interests of all involved parties.
Constitution's Journey: From Idea to Law
You may want to see also

Cash payments
In some countries, compensated organ donation is permitted and regulated by the government. For example, Iran allows living donors to receive reasonable compensation for donating a kidney. Similarly, India and Pakistan permit the sale of human organs, often with poor individuals selling their organs to wealthier recipients. However, this practice raises ethical and legal concerns related to exploitation and inequality.
In the United States, the National Organ Transplant Act (NOTA) prohibits the transfer of human organs "for valuable consideration" for transplantation. However, there is ongoing debate about providing financial incentives for living donors to increase the availability of organs. Some proposals focus on reimbursing donors for expenses incurred during the donation process, including travel, housing, and lost wages. While removing financial disincentives is allowed under NOTA, introducing financial incentives would require careful consideration of economic, legal, ethical, and public readiness factors.
Proponents of cash payments argue that the current altruistic system cannot meet the growing demand for transplantable organs. They suggest that compensating donors could motivate more people to donate. Dr. Sally Satel, a kidney transplant recipient, supports rewarding donors as a way to address the critical organ shortage. She proposes state or federally provided payments, such as tax credits, tuition vouchers, or Medicare vouchers, to compensate donors fairly without encouraging impulsive decisions by those in financial need.
While cash payments for organ donation can be controversial, some argue that it is similar to other accepted practices, such as selling blood or plasma. Additionally, supporters of compensation highlight the potential to save lives by increasing the availability of organs for those awaiting transplants. However, it is essential to carefully navigate the ethical and legal complexities to ensure that any form of compensation is implemented ethically and responsibly.
Martial Law and Double Jeopardy: A Court's Decision
You may want to see also

Tax deductions
One argument in favour of tax deductions as a form of compensation is that it removes financial disincentives for living donors. Currently, donors may incur various expenses during the evaluation, surgery, and aftercare processes. These expenses may include travel costs, housing, and lost wages. By offering tax deductions, donors can be reimbursed for these expenses, making the act of donation financially neutral. This approach is supported by the transplant community, which seeks to remove disincentives without providing direct financial incentives that could raise ethical concerns.
In some countries, compensated organ donation is legal and ethically regulated. For example, Iran has a government-regulated program that ensures living donors receive reasonable compensation for donating a kidney. However, in countries where the sale of organs is permitted, such as India and Pakistan, ethical concerns have been raised regarding the exploitation of poor donors by wealthier recipients.
To address these ethical concerns, experts like Dr. Sally Satel have proposed forms of compensation that would not exploit vulnerable populations. Instead of immediate cash payments, Dr. Satel suggests state or federally provided payments such as tax credits, tuition vouchers, 401(k) contributions, or Medicare vouchers. These forms of compensation would fairly compensate donors without encouraging hasty or dangerous decisions driven by financial desperation.
While the debate around compensating organ donors continues, tax deductions and other forms of financial incentives are being considered as potential solutions to increase organ availability and reduce waiting times for transplants. However, it is essential to carefully evaluate the economic, legal, ethical, and social implications of any policy changes to ensure equitable and ethical organ donation practices.
Blood Loss: Understanding the Threshold of Life-Threatening Injuries
You may want to see also
Explore related products

Priority access for family members
Firstly, defining "family members" can be challenging due to varying family structures and relationships. Deciding who qualifies as a family member for priority access could lead to disputes and ethical dilemmas. For example, should priority access extend to distant relatives or only immediate family members? What about adopted family members or those without legal ties but strong emotional connections? These questions highlight the complexity of defining family relationships and the potential for controversy.
Secondly, offering priority access to family members of organ donors could inadvertently create a two-tiered system, where individuals with donor family members gain an advantage over others in need of transplants. This could further exacerbate existing inequalities and result in an unfair distribution of organs. It is crucial to ensure that organ allocation remains equitable and based on medical need rather than the donor status of family members.
Thirdly, the logistics of implementing such a system could be challenging. Prioritizing family members of organ donors across multiple transplant waiting lists might require complex coordination between various healthcare institutions and organizations. Ensuring that priority access is granted fairly and consistently across the board would necessitate a high level of organization and collaboration.
However, it is important to acknowledge that providing priority access to family members of organ donors could serve as a form of recognition and gratitude for their selfless act. It could be argued that offering priority access in cases of future organ transplants for family members is a meaningful way to compensate for their generosity and potentially encourage more people to become donors.
Lastly, while priority access for family members may be considered, it should not be the sole or primary form of compensation. As highlighted by Singapore's health minister, Khaw Boon Wan, it is crucial to explore "meaningful compensation" that does not breach ethical principles. This could include reimbursement of expenses, lost wages, childcare and eldercare costs, and other forms of financial support to ensure that organ donation does not create a financial burden for donors and their families.
In conclusion, while priority access for family members of organ donors may be considered as part of a comprehensive compensation strategy, it should be approached with caution and careful ethical, legal, and logistical considerations. The focus should be on providing meaningful compensation that respects donors, supports their well-being, and does not inadvertently create inequalities or complexities in the organ allocation system.
God's Influence in the US Constitution: A Religious Exploration
You may want to see also

Reimbursement of expenses
While organ donors are not typically compensated for their donation, some countries and states provide some form of compensation. The National Organ Transplant Act (NOTA) prohibits the transfer of human organs for 'valuable consideration', but allows for the removal of financial disincentives.
Some have argued that reimbursement of expenses alone is not sufficient to address the shortage of organs available for transplant. Instead, financial incentives may be necessary to motivate more people to become donors. However, the idea of providing financial incentives for organ donation has raised ethical concerns, particularly around the potential exploitation of vulnerable individuals.
To address these concerns, alternative forms of compensation have been proposed, such as state or federally provided payments like tax credits, tuition vouchers, or Medicare vouchers. These forms of compensation aim to fairly compensate donors without encouraging hasty or dangerous decisions.
Overall, the reimbursement of expenses for organ donors is a complex issue that requires careful consideration of ethical, legal, and economic factors to ensure that donors are adequately supported without exploiting vulnerable individuals.
The Supreme Court: How Many Members Constitute It?
You may want to see also
Frequently asked questions
Meaningful compensation for organ donors can take various forms, including cash payments, tax deductions, priority access to organs for their family members, or reimbursement of expenses incurred during the donation process. Some countries provide donors with compensation, while others believe that organ donation should be an altruistic act.
The controversy surrounding compensation for organ donors stems from ethical concerns about the potential exploitation of vulnerable individuals, particularly the poor and desperate. There is a fear that allowing financial incentives for organ donation could lead to dangerous procedures and undermine the spirit of selflessness associated with organ donation.
Advocates for compensating organ donors argue that it could help address the dire shortage of organs available for transplantation. By providing financial incentives, more people might be motivated to become donors, increasing the likelihood of matching organs with those in need.
To balance the need for organs with ethical concerns, some have suggested forms of compensation that would not exploit vulnerable individuals. For example, Dr. Sally Satel proposes state or federally provided payments such as tax credits, tuition vouchers, or Medicare vouchers. These forms of compensation fairly recognise donors without encouraging hasty or dangerous decisions.