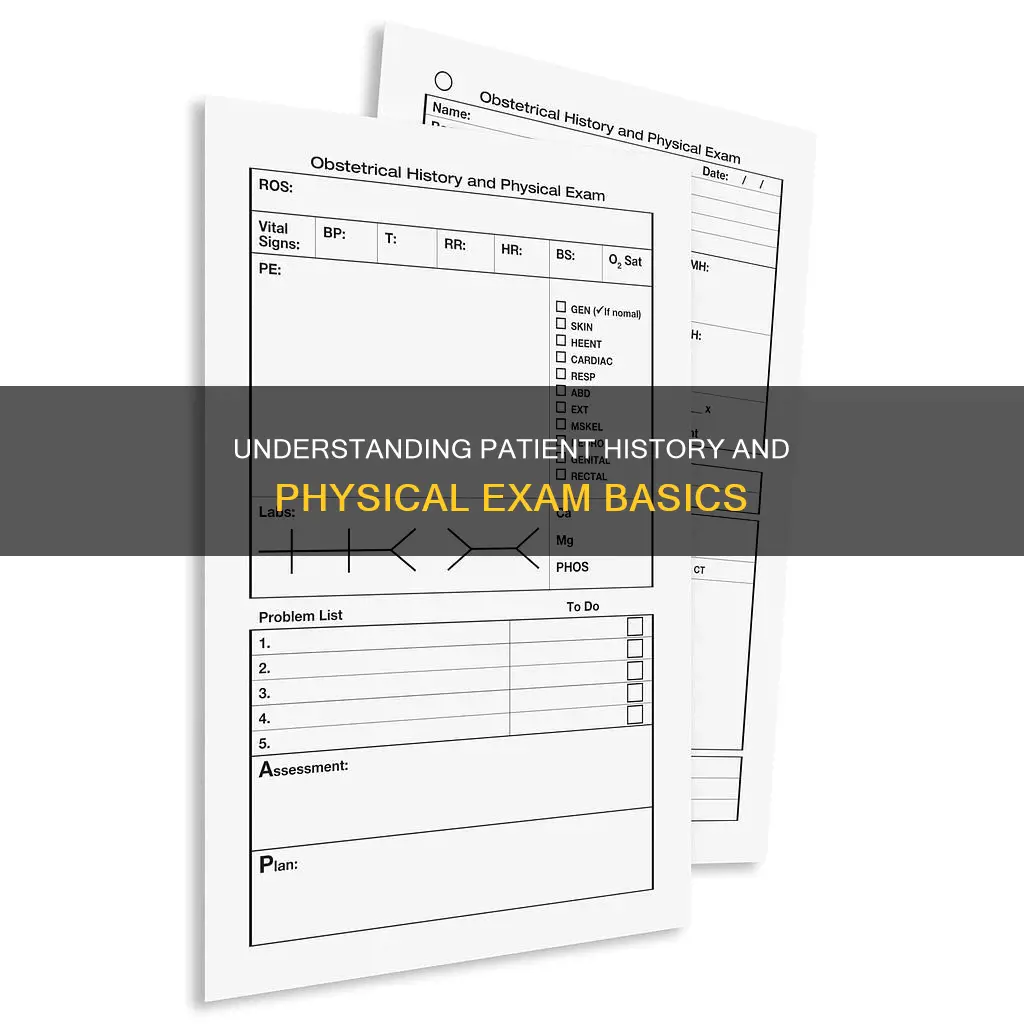
A patient's history and physical examination are crucial components of medical practice, providing essential information for diagnosis, treatment, and patient management. The history component involves gathering a patient's medical history, including their present and past illnesses, family and social history, allergies, medications, and other relevant details. This information aids in making differential diagnoses and determining potential health risks. The physical examination involves a thorough assessment of the patient's physical state, including observations of their appearance, skin colouration, gait, and other indicators that can provide valuable insights into their overall health. Together, the history and physical examination form the foundation for developing a treatment plan and managing the patient's care. The initial consultation is particularly important, as it sets the tone for the patient-physician relationship and guides further diagnostic investigations and management strategies.
| Characteristics | Values |
|---|---|
| Time allocated | Hospital consultants may allow up to an hour for new patient consultations, whereas general practice usually allocates 10 minutes. |
| Purpose | To gather information on the patient's education, social background, and physical signs. |
| Techniques | Observation of the patient's facies, skin colouration, gait, handshake, and personal hygiene. |
| Medical History | Present illness, past medical conditions, family medical history, social history, allergies, and medications. |
| Chief Complaint | Written in the patient's own words and explored in detail. |
| Patient Understanding | Ensure patients understand questions and can provide accurate histories based on their health literacy. |
| Language Barriers | Use facility-provided language services to assist with communication. |
| Record-Keeping | Proofreading is essential to avoid errors in electronic prescriptions and medical records. |
| Practitioner Qualifications | Completed and documented by a qualified and privileged physician or other licensed practitioner, such as nurse practitioners or physician assistants. |
| Authentication | Each entry must be signed, dated, and timed by the author. |
| Surgery Requirements | A comprehensive medical history and physical examination are required before high-risk procedures, surgical procedures, and procedures involving anesthesia. |
Explore related products
What You'll Learn

Medical history
A patient's medical history is a comprehensive record that lists all illnesses and treatments they have had. It is a set of information collected by physicians through medical interviews. It is typically the first contact between the physician and the patient and plays a crucial role in diagnosis and treatment planning.
The medical history can reveal diagnosed medical conditions, past medical issues, and potential future health risks. It includes the patient's past illnesses, surgeries, medication responses, and recovery patterns. It also covers familial medical history, allergies, lifestyle, living conditions, and profession. For example, in the case of a patient with a history of bariatric surgery, there may be an underlying diagnosis of hyperlipidemia. Additionally, for women, it is essential to inquire about previous pregnancies, abortions, or miscarriages, as these can impact treatment options and imaging modalities.
The social history component of a medical record can vary depending on the clinician's values and scope of practice. It may include substance use, nutrition, travel history, and living arrangements. For instance, recent travel history could be crucial for emergency medicine clinicians, as failing to ask about it could exclude a diagnosis of meningitis.
In certain cases, such as with geriatric patients, immunization status and medication interactions are important considerations. For surgical specialties, a detailed history of previous surgeries is vital for planning future procedures. A patient's medical history can also help identify patterns even before symptoms appear. For example, a history of severe heartburn could warrant investigations for GERD, even in the absence of current symptoms.
Overall, a patient's medical history is a dynamic and detailed account that guides healthcare professionals in making accurate diagnoses, personalizing treatment plans, and predicting future health risks.
Malevolent Armor Requirements: Do You Need Constitution?
You may want to see also

Physical examination
A physical examination is a process of evaluating a patient's objective anatomic findings through observation, palpation, percussion, and auscultation. The examination methods can vary depending on the patient's age and the reason for their appointment. It is often a yearly check-up to evaluate a patient's overall health and address any concerns they may have.
During a physical examination, a medical practitioner will ask the patient a series of questions about their medical history and symptoms, followed by an examination based on the reported symptoms. The medical history and physical examination help determine a diagnosis and treatment plan. The patient's data then becomes part of their medical record.
The examination can include checking the patient's height, weight, blood pressure, and vision and hearing. The provider may also examine the patient's flexibility and strength. The patient's skin may be examined for any unusual moles, rashes, or other concerns. The provider may also use a stethoscope to listen to the patient's heart and lungs and check the lymph nodes in the neck for swelling.
In some cases, further testing may be required, such as blood tests, complete blood count (CBC), electrocardiogram (EKG), stress test, urinalysis, or a lipid panel. If there are concerns after the physical exam, the provider may request additional appointments to monitor the results and ensure the patient's health.
Presidential Roles: Two Unconstitutional Powers Explored
You may want to see also

Patient's story
A physical examination is an important aspect of a patient's overall health evaluation and can provide valuable insights that technological scans and tests might miss. During a physical exam, the patient's story or medical history is crucial, as it offers context and helps guide the examination.
The patient's story begins with a detailed account of their current health status, including any symptoms they are experiencing. This narrative often starts with a description of any concerns or problems the patient is facing, such as pain, discomfort, or unusual observations they have noticed. For example, a patient may report a persistent cough, unexplained weight loss, or changes in their energy levels. It is important for the patient to describe these symptoms in detail, including when they first appeared, their frequency, duration, and any factors that seem to trigger or alleviate them.
In addition to current symptoms, the patient's story also encompasses their medical history. This includes information about any previous illnesses, injuries, surgeries, or treatments. For example, a patient may have a history of asthma, a previous broken bone, or a family history of heart disease. Providing a comprehensive medical history helps to paint a clearer picture of the patient's overall health and can often provide valuable clues about their current condition.
During the patient's story, it is also essential to discuss any medications or supplements they are currently taking or have taken in the past. This includes prescriptions, over-the-counter drugs, herbal remedies, and vitamins. By understanding a patient's medication history, healthcare providers can identify potential side effects, interactions, or allergies that may impact their health and influence the interpretation of physical examination findings.
Furthermore, the patient's story should include their social history, such as their occupation, living situation, and any relevant lifestyle factors. For example, a patient's job may involve physical labour or exposure to potential health hazards. Their living situation may impact their access to healthy food or their ability to manage stress. Discussing lifestyle factors such as diet, exercise habits, substance use, and sleep patterns can also provide valuable insights into their overall health and areas where modifications may be beneficial.
The patient's story is a critical component of the physical examination as it allows healthcare providers to individualize the examination, focusing on areas of concern and considering the patient's unique context. By listening attentively to the patient's narrative, healthcare providers can develop a more holistic understanding of their health, guide the direction of the physical exam, and ultimately, provide more personalized care and treatment recommendations.
Understanding Board Fees: Trade or Business?
You may want to see also
Explore related products

Diagnostic tests
The patient's medical history is considered the most useful element in making an accurate diagnosis, even more so than diagnostic tests or physical examinations. During the interview, the physician must be attentive to the patient's story, body language, and responses to form a preliminary diagnosis and differential diagnoses. The accuracy of the medical interview depends on the physician's ability to ask pertinent questions and the patient's accurate recall of their symptoms.
In addition to medical history, a psychosocial history may also be taken, including information on education, lifestyle, marital status, religious beliefs, smoking history, alcohol intake, and use of controlled substances. This information can influence future medical decisions. The patient's current medication, over-the-counter remedies, and supplements are also noted, as these can contribute to the patient's current problem or influence the choice of medication.
The Free Will Defense: A Sound Theodicy?
You may want to see also

Qualified practitioners
For qualified practitioners, a patient's history and physical examination are crucial components of providing effective care. The history and physical (H&P) involve gathering a comprehensive understanding of the patient's health, including their medical history, social background, and physical condition. This process is essential for accurate diagnosis, treatment planning, and patient management.
During the initial patient encounter, qualified practitioners must pay close attention to the patient's story, observing both verbal and non-verbal cues. This information gathering process allows practitioners to form preliminary diagnoses and differential diagnoses, as well as to build trust and rapport with the patient. It is important to ensure that patients understand questions and feel comfortable providing accurate information. This may involve using colloquial terms, addressing patient concerns, and reassuring patients about the purpose of information gathering.
The physical examination component of the H&P involves a thorough assessment of the patient's physical condition. This may include examining the patient's cardiovascular or respiratory system, but it also extends beyond physical observations. Qualified practitioners should also consider the patient's psychological and social background, including factors such as personal hygiene, which can provide valuable insights.
In some cases, the H&P may be performed by multiple qualified practitioners, each contributing their expertise. For example, a dentist or podiatrist may perform aspects of the H&P relevant to their specialty. Additionally, in cases where the patient is unable to provide a clear history, family members or caregivers may provide valuable information. The H&P should be authenticated and entered into the patient's medical record in a timely manner, typically within 30 days, to ensure compliance and continuity of care.
Quoting Authors: New Paragraphs or Not?
You may want to see also
Frequently asked questions
The purpose is to gather information to diagnose and manage the patient's illness and to form a relationship with the patient.
A patient history includes the patient's medical history, past surgical history, family medical history, social history, allergies, and medications.
The physician must be attentive to the patient's story, piecing together each bit of evidence to form a tentative preliminary diagnosis and differential diagnoses.
There is no clear dividing line between history and examination. During the course of the history, information on the patient's education and social background is gathered, and to a lesser extent, there will be physical signs to pick up.
The process involves taking a careful and complete history and performing a thorough physical examination. This includes observing the patient's facies, skin colouration, gait, handshake, and personal hygiene.


















![McKesson Disposable Patient Exam Gown [Pack of 50] Latex-Free, Medical, Hospital, Tissue/Polyester, Blue, One Size Fits Most](https://m.media-amazon.com/images/I/71daP5mjSvL._AC_UY218_.jpg)
























