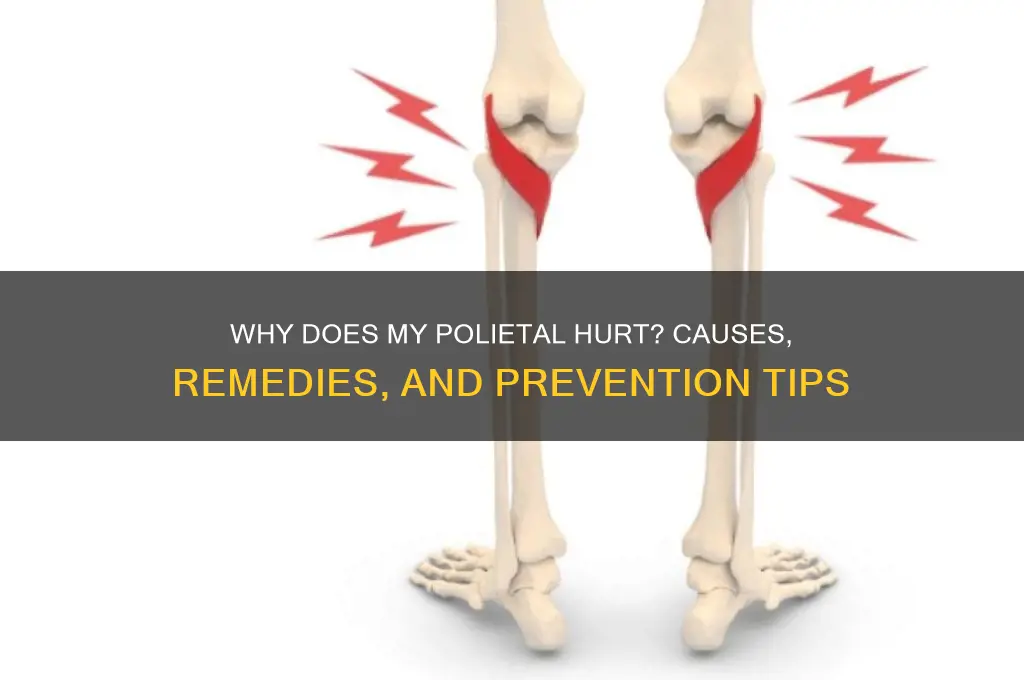
Politeal pain, often referring to discomfort in the bursa located near the hip joint, can stem from various factors such as inflammation, overuse, injury, or underlying conditions like bursitis or tendonitis. This pain may manifest as a dull ache, sharp discomfort, or stiffness, particularly during movement or prolonged activity. Understanding the root cause is crucial for effective management, which may involve rest, physical therapy, anti-inflammatory medications, or, in severe cases, medical intervention. Addressing politeal pain promptly can prevent further complications and restore mobility and comfort.
Explore related products
What You'll Learn
- Common Causes: Overuse, injury, or underlying conditions like arthritis can cause politeal pain
- Symptoms to Watch: Swelling, redness, or limited mobility may indicate a serious politeal issue
- Prevention Tips: Proper posture, regular stretching, and ergonomic adjustments can reduce politeal strain
- When to See a Doctor: Persistent pain, numbness, or weakness requires immediate medical attention?
- Treatment Options: Rest, physical therapy, medications, or surgery may alleviate politeal discomfort

Common Causes: Overuse, injury, or underlying conditions like arthritis can cause politeal pain
Common Causes: Overuse, Injury, or Underlying Conditions Like Arthritis Can Cause Popliteal Pain
One of the most frequent causes of popliteal (behind-the-knee) pain is overuse, particularly in individuals who engage in repetitive activities that strain the knee joint. Athletes, runners, cyclists, or even individuals with physically demanding jobs often experience this type of pain due to excessive stress on the muscles, tendons, and ligaments surrounding the popliteal area. Over time, this repetitive motion can lead to inflammation, tendonitis, or bursitis, causing discomfort or sharp pain behind the knee. Rest, ice, and physical therapy are often recommended to alleviate symptoms and prevent further damage.
Injury is another common culprit behind popliteal pain. Direct trauma, such as a fall or blow to the knee, can result in sprains, strains, or even fractures that affect the popliteal region. Additionally, injuries to the ligaments or tendons, like a torn meniscus or hamstring strain, can radiate pain to the back of the knee. In some cases, a Baker’s cyst—a fluid-filled swelling caused by knee joint issues—may develop, leading to popliteal pain and stiffness. Immediate medical evaluation is crucial for injuries to determine the extent of damage and appropriate treatment, which may include immobilization, medication, or surgery.
Underlying conditions like arthritis frequently contribute to popliteal pain, especially in older adults or those with a history of joint issues. Osteoarthritis, rheumatoid arthritis, and gout can cause inflammation and degeneration of the knee joint, leading to pain, swelling, and reduced mobility in the popliteal area. Arthritis-related pain often worsens with activity and may be accompanied by stiffness, particularly in the morning or after prolonged rest. Managing arthritis typically involves a combination of pain relief medications, lifestyle modifications, and, in severe cases, joint replacement surgery.
It’s important to note that popliteal pain can also arise from referred pain, where the source of discomfort is not the knee itself but another area, such as the lower back or hip. Conditions like sciatica or herniated discs can cause nerve compression that radiates pain to the back of the knee. Similarly, deep vein thrombosis (DVT), a blood clot in the leg, may present as popliteal pain along with swelling, warmth, and redness. If pain is accompanied by severe swelling, difficulty walking, or sudden onset, immediate medical attention is necessary to rule out serious conditions like DVT.
Lastly, poor posture or biomechanics can indirectly lead to popliteal pain by placing uneven stress on the knee joint. Misalignment in the hips, ankles, or feet can alter gait and weight distribution, overloading the structures behind the knee. Custom orthotics, physical therapy, and corrective exercises can help address these issues and reduce strain on the popliteal area. Understanding the root cause of the pain is essential for effective treatment, so consulting a healthcare professional for a thorough evaluation is always recommended.
HSUS Political Affiliations: Uncovering Ties to Parties and Ideologies
You may want to see also

Symptoms to Watch: Swelling, redness, or limited mobility may indicate a serious politeal issue
When experiencing pain in the popliteal area (the back of the knee), it’s crucial to monitor for specific symptoms that may signal a serious underlying issue. Swelling is one of the most noticeable signs to watch for. If the area behind your knee appears larger than usual or feels tight, it could indicate inflammation, a cyst (like a Baker’s cyst), or even a blood clot. Swelling that persists or worsens over time warrants immediate medical attention, as it may suggest a condition requiring prompt treatment.
Redness in the popliteal region is another symptom that should not be ignored. While mild redness might be due to minor irritation or friction, intense or spreading redness could be a sign of infection or inflammation. For instance, cellulitis, a bacterial skin infection, can cause redness, warmth, and pain in the affected area. If redness is accompanied by fever, chills, or streaks extending from the knee, seek medical care urgently, as these could indicate a severe infection or blood-related issue.
Limited mobility is a critical symptom that may point to a serious popliteal problem. If you find it difficult to bend or straighten your knee, or if movement causes sharp pain, it could be due to a structural issue like a torn meniscus, tendon injury, or even a popliteal cyst compressing nearby structures. Limited mobility can also result from swelling or inflammation within the joint. Ignoring this symptom may lead to further damage or chronic pain, so consulting a healthcare professional is essential for proper diagnosis and treatment.
In addition to these symptoms, persistent or worsening pain in the popliteal area should be taken seriously. Pain that does not improve with rest, ice, or over-the-counter pain relievers may indicate a deeper issue, such as a nerve compression, artery problem, or even a tumor. If the pain is severe, radiating, or accompanied by numbness or tingling, it could suggest nerve involvement, requiring specialized care.
Lastly, visible deformity or unusual lumps in the popliteal region should raise concern. A Baker’s cyst, for example, can cause a noticeable bulge behind the knee, while a blood clot or aneurysm might present as a firm, tender mass. Any abnormal growth or change in the area’s appearance should be evaluated by a healthcare provider to rule out serious conditions. Monitoring these symptoms and acting promptly can prevent complications and ensure appropriate management of popliteal pain.
Can Political Parties Be Banned? Legal and Ethical Implications Explored
You may want to see also

Prevention Tips: Proper posture, regular stretching, and ergonomic adjustments can reduce politeal strain
Preventing Politeal Pain Through Proper Posture
Maintaining proper posture is essential for reducing strain on the politeal area, which includes the back of the knee and surrounding structures. Poor posture, especially when sitting or standing for long periods, can place undue stress on this region. To prevent discomfort, ensure your spine is aligned naturally when sitting—keep your feet flat on the floor, shoulders relaxed, and ears aligned with your shoulders. Avoid slouching or leaning forward, as this can tighten the muscles around the politeal area. When standing, distribute your weight evenly on both legs and avoid locking your knees, which can restrict blood flow and increase tension. Consistently practicing good posture throughout the day can significantly minimize the risk of politeal pain.
Incorporate Regular Stretching into Your Routine
Regular stretching is a powerful tool to alleviate and prevent politeal strain. Tight muscles in the hamstrings, calves, and quadriceps can pull on the politeal area, leading to discomfort. Incorporate dynamic stretches like leg swings and static stretches like hamstring stretches into your daily routine. Hold each stretch for 20–30 seconds, focusing on gentle tension rather than pain. Stretching after prolonged periods of sitting or standing can help maintain flexibility and reduce muscle tightness. Additionally, yoga or Pilates exercises that target the lower body can improve overall muscle balance and reduce strain on the politeal region.
Ergonomic Adjustments for Politeal Health
Ergonomic adjustments in your workspace and daily activities can play a crucial role in preventing politeal pain. If you work at a desk, ensure your chair is adjusted to a height where your knees are level with your hips, and your feet are firmly planted on the ground. Use a footrest if necessary to avoid dangling feet, which can strain the back of the knees. Position your monitor at eye level to prevent leaning forward, and keep frequently used items within arm’s reach to minimize twisting or overextending. For those who stand for long periods, use anti-fatigue mats and alternate between sitting and standing to reduce pressure on the politeal area.
Mindful Movement and Activity Modifications
Being mindful of how you move during physical activities can prevent politeal strain. Avoid sudden, jerky movements that can overextend the muscles and tendons around the knee. When exercising, warm up properly and choose low-impact activities like swimming or cycling if you’re prone to politeal discomfort. If your job involves heavy lifting or repetitive motions, use proper techniques to avoid putting excessive stress on the knees. Wearing supportive footwear with adequate cushioning can also reduce impact on the politeal area during walking or standing.
Hydration and Muscle Recovery
While not directly related to posture or ergonomics, staying hydrated and prioritizing muscle recovery can indirectly prevent politeal strain. Dehydration can lead to muscle stiffness, increasing the likelihood of strain. Drink plenty of water throughout the day, especially if you’re physically active. After exercise or a long day of standing, apply ice or heat to the politeal area to reduce inflammation and promote relaxation. Pairing these practices with proper posture, stretching, and ergonomic adjustments creates a comprehensive approach to preventing politeal pain and maintaining overall lower body health.
Does Massachusetts Mandate Political Parties for Primary Elections?
You may want to see also
Explore related products

When to See a Doctor: Persistent pain, numbness, or weakness requires immediate medical attention
If you're experiencing persistent pain, numbness, or weakness in your sciatic nerve area, often referred to as sciatica, it’s crucial to understand when these symptoms warrant immediate medical attention. Sciatica occurs when the sciatic nerve, which runs from the lower back down the legs, is compressed or irritated. While occasional discomfort may resolve on its own, persistent or worsening symptoms should not be ignored. If the pain is severe, unrelenting, or accompanied by progressive weakness in the leg or foot, it’s a clear sign to consult a doctor. These symptoms could indicate a more serious underlying condition, such as a herniated disc, spinal stenosis, or even a tumor, which requires prompt evaluation and treatment.
Numbness or tingling in the leg or foot is another red flag that should prompt a visit to the doctor. While occasional numbness might be harmless, persistent or spreading numbness could signal nerve damage or compression that needs immediate attention. If you notice a loss of sensation or difficulty moving your leg or foot, it’s essential to seek medical care. Ignoring these symptoms can lead to long-term nerve damage or permanent disability, especially if the cause is a severe condition like cauda equina syndrome, a rare but serious disorder affecting the nerves at the lower end of the spinal cord.
Weakness in the leg or foot is a symptom that should never be overlooked. If you find it difficult to lift your foot, walk, or maintain balance, this could indicate significant nerve or muscle impairment. Weakness often suggests that the sciatic nerve is being compressed to the point where it affects muscle function. Conditions like lumbar spinal stenosis or a large herniated disc can cause such symptoms, and delaying treatment may result in irreversible damage. A doctor can perform tests like MRI or CT scans to identify the cause and recommend appropriate interventions, such as physical therapy, medication, or surgery.
It’s also important to seek medical attention if your pain is accompanied by other concerning symptoms, such as fever, unexplained weight loss, or bladder or bowel incontinence. These could be signs of an infection, inflammation, or a more systemic issue that requires urgent care. Additionally, if your pain follows a traumatic injury, such as a fall or accident, immediate evaluation is necessary to rule out fractures or other structural damage. Early intervention can prevent complications and improve outcomes, so don’t hesitate to contact a healthcare professional if you’re unsure about the severity of your symptoms.
Lastly, if home remedies like rest, ice, heat, or over-the-counter pain relievers fail to alleviate your symptoms after a week or two, it’s time to see a doctor. Persistent pain, numbness, or weakness that interferes with daily activities or sleep is not normal and should be addressed professionally. A doctor can provide a thorough assessment, diagnose the underlying cause, and create a tailored treatment plan to relieve your discomfort and prevent further issues. Remember, timely medical attention can make a significant difference in managing sciatic nerve pain and ensuring long-term health.
Did People Want Political Parties? Exploring the Origins and Public Sentiment
You may want to see also

Treatment Options: Rest, physical therapy, medications, or surgery may alleviate politeal discomfort
When addressing politeal (popliteal) pain, the treatment approach depends on the underlying cause, which could range from muscle strain to cysts, nerve compression, or vascular issues. Rest is often the first line of treatment, especially if the pain is due to overuse or injury. Avoiding activities that exacerbate the discomfort allows the affected area to heal. Elevating the leg and applying ice packs can reduce inflammation and alleviate pain. It’s crucial to listen to your body and avoid putting excessive pressure on the knee or overusing the muscles in the popliteal region until the pain subsides.
Physical therapy is another effective treatment option, particularly for pain caused by muscle imbalances, tightness, or poor posture. A physical therapist can design a tailored exercise program to strengthen the surrounding muscles, improve flexibility, and correct movement patterns that may be contributing to the pain. Stretching exercises for the hamstrings, calves, and quadriceps can relieve tension in the popliteal area. Additionally, techniques like manual therapy or ultrasound may be used to promote healing and reduce discomfort.
Medications may be recommended to manage pain and inflammation. Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, can help reduce swelling and relieve pain. For more severe cases, a healthcare provider might prescribe stronger pain relievers or corticosteroid injections to target inflammation directly. However, medications should be used under medical supervision, as prolonged use can have side effects.
In cases where conservative treatments fail to provide relief, surgery may be considered. This is typically reserved for structural issues like popliteal cysts (Baker’s cysts), nerve entrapment, or vascular problems. For example, a cyst that causes persistent pain or limits mobility may need to be drained or surgically removed. Similarly, if a compressed nerve or blood vessel is the root cause, surgical intervention may be necessary to decompress or repair the affected area. Surgery is usually a last resort and is followed by a period of rehabilitation to ensure full recovery.
It’s essential to consult a healthcare professional for an accurate diagnosis before pursuing any treatment. They can determine the cause of the popliteal pain and recommend the most appropriate approach, whether it’s rest, physical therapy, medications, or surgery. Early intervention can prevent complications and restore comfort and function to the affected area.
Unveiling Deception: Why Political Leaders Resort to Lying
You may want to see also
Frequently asked questions
Prolonged sitting can compress the piriformis muscle, leading to tightness and irritation. This can cause pain in the buttock area and may radiate down the leg, often referred to as piriformis syndrome.
Repetitive activities like running or exercising can overwork the piriformis muscle, causing strain or inflammation. Poor biomechanics or muscle imbalances may also contribute to the pain.
Walking or climbing stairs engages the piriformis muscle, and if it’s tight, weak, or irritated, it can cause pain. This discomfort may be a sign of piriformis syndrome or related issues like sciatic nerve compression.
Persistent piriformis pain at rest could indicate chronic inflammation, muscle spasms, or underlying conditions like a herniated disc or sciatica. It’s advisable to consult a healthcare professional for proper diagnosis and treatment.