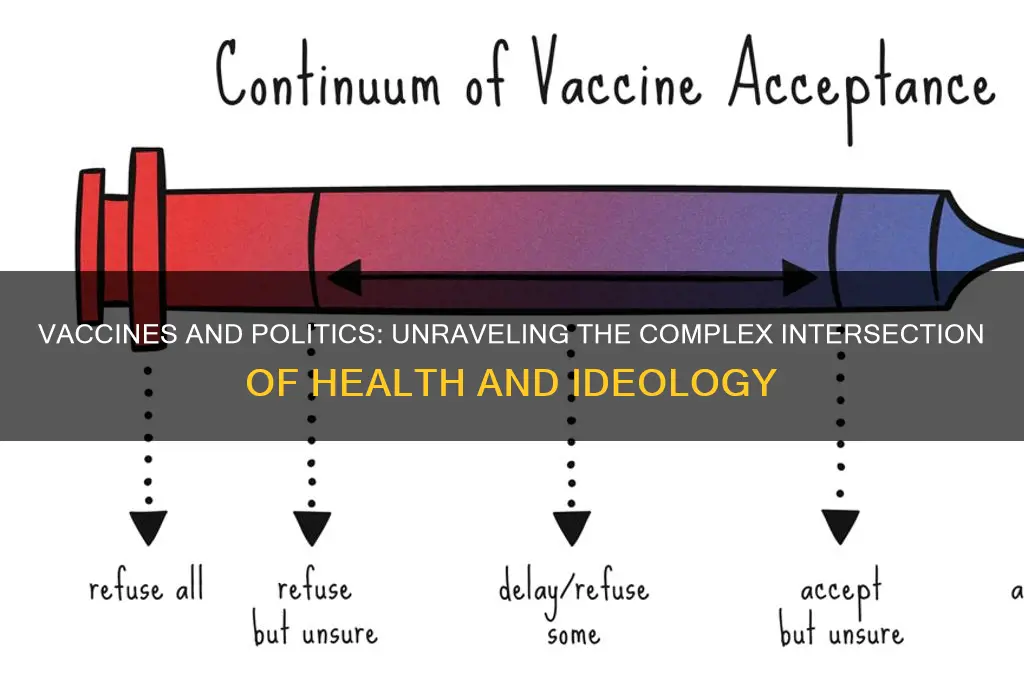
Vaccines have become increasingly politicized in recent years, transforming from a public health issue into a contentious political debate. This shift can be attributed to a combination of factors, including misinformation spread through social media, distrust in government and scientific institutions, and the alignment of vaccine mandates with partisan ideologies. Political leaders and media outlets often frame vaccination policies as encroachments on personal freedom, while public health experts emphasize their role in preventing disease and protecting communities. Additionally, historical and cultural contexts, such as past medical injustices in marginalized communities, have fueled skepticism and resistance. As a result, vaccine policies have become a battleground in broader political conflicts, complicating efforts to achieve widespread immunization and combat preventable diseases.
| Characteristics | Values |
|---|---|
| Historical Mistrust | Past medical abuses (e.g., Tuskegee Syphilis Study) fuel skepticism. |
| Political Polarization | Vaccine mandates became a partisan issue during COVID-19 (e.g., U.S. divide). |
| Misinformation Spread | Social media amplifies false claims (e.g., autism link, microchips). |
| Individual vs. Collective Rights | Debates over personal freedom vs. public health mandates. |
| Corporate Influence | Pharma lobbying and profit motives raise ethical concerns. |
| Global Inequity | Vaccine hoarding by wealthy nations during COVID-19 (e.g., COVAX struggles). |
| Religious/Cultural Beliefs | Opposition based on religious or cultural grounds (e.g., halal/kosher concerns). |
| Government Overreach Perception | Mandates seen as state overreach by libertarian groups. |
| Scientific Skepticism | Distrust in rapid vaccine development (e.g., mRNA technology doubts). |
| Economic Impact | Vaccine passports affecting livelihoods (e.g., job losses for unvaccinated). |
| Celebrity/Influencer Influence | High-profile figures spreading anti-vaxx narratives (e.g., Robert F. Kennedy Jr.). |
| Regulatory Transparency Concerns | Questions about FDA/WHO approval processes during emergencies. |
| Colonialism Legacy | Historical exploitation in developing nations fuels vaccine hesitancy. |
| Mandate Enforcement | Legal battles over school/workplace mandates (e.g., U.S. Supreme Court cases). |
| Data Privacy Fears | Concerns about vaccine passports linking to personal data. |
Explore related products
What You'll Learn
- Historical mistrust in government health initiatives fuels vaccine skepticism
- Political polarization amplifies vaccine debates as partisan issues
- Corporate influence on vaccine development raises public suspicion
- Mandatory vaccine policies clash with individual freedom arguments
- Global vaccine distribution inequity sparks political tensions

Historical mistrust in government health initiatives fuels vaccine skepticism
The roots of vaccine skepticism often trace back to a deep-seated historical mistrust in government health initiatives, particularly within marginalized communities. One of the most cited examples is the Tuskegee Syphilis Study (1932–1972), where the U.S. Public Health Service deliberately withheld treatment from African American men with syphilis, even after penicillin became the standard cure. This egregious violation of ethical standards left a lasting legacy of distrust among Black Americans toward government-led health programs. Such historical injustices have created a fertile ground for skepticism, making it difficult for public health messages about vaccines to be accepted without question.
Another instance of government overreach that fuels mistrust is the forced sterilization programs in the early 20th century, particularly targeting Indigenous, Black, and immigrant women in the United States. These programs, often justified under the guise of public health and eugenics, were carried out without informed consent and violated the bodily autonomy of thousands of individuals. Such actions have ingrained a skepticism toward government interventions, especially when they involve medical procedures like vaccination. This historical context is crucial for understanding why some communities view vaccine mandates or recommendations with suspicion.
Globally, similar patterns of mistrust can be observed in former colonial nations. In countries like Nigeria and India, colonial-era medical experiments and forced vaccinations have left a lingering skepticism toward Western-developed vaccines. For example, rumors during the polio eradication campaign in Nigeria in the early 2000s suggested that the vaccine was a Western plot to sterilize Muslim girls, leading to widespread refusal. These rumors were not baseless but were rooted in historical experiences of exploitation by colonial powers, which continue to shape perceptions of government health initiatives today.
The Cold War era also contributed to vaccine politicization, particularly through the lens of propaganda and ideological battles. In the Soviet Union, for instance, government-led health campaigns were often viewed as tools of state control rather than genuine public health efforts. Similarly, in the West, anti-communist sentiments sometimes led to skepticism of government programs, including vaccination drives. This ideological divide further entrenched the idea that health initiatives could be weaponized, fostering a climate of distrust that persists in various forms today.
Finally, the historical misuse of medical research during wartime, such as Japan’s Unit 731 during World War II, where horrific human experimentation was conducted under the guise of medical research, has also contributed to global mistrust. These atrocities, though not directly related to vaccines, have created a broader skepticism of state-sponsored medical interventions. When governments promote vaccines, especially during crises like the COVID-19 pandemic, this historical mistrust resurfaces, making it challenging to achieve widespread acceptance. Understanding this history is essential for addressing vaccine skepticism and rebuilding trust in public health initiatives.
Can Political Parties Legally Remove Their Own Members from Office?
You may want to see also

Political polarization amplifies vaccine debates as partisan issues
Political polarization has transformed vaccine debates into deeply partisan issues, exacerbating public health challenges. In recent decades, vaccines, once universally accepted as a cornerstone of public health, have become entangled in ideological divides. This shift is largely driven by the broader trend of political polarization, where issues that were previously non-partisan are now viewed through a lens of "us versus them." For instance, during the COVID-19 pandemic, vaccine mandates and public health measures became flashpoints, with political affiliations often predicting one’s stance on vaccination. This polarization is not merely a reflection of differing opinions but a symptom of how political identities shape beliefs, even on matters of science and health.
One key factor amplifying this polarization is the role of political leaders and media outlets in framing vaccine debates. Politicians often leverage vaccine issues to rally their base, portraying mandates as either essential for public safety or as government overreach, depending on their party’s stance. For example, in the U.S., Republican and Democratic leaders have frequently taken opposing positions on vaccine mandates, with conservative figures often emphasizing individual liberty and Democrats stressing collective responsibility. This partisan framing trickles down to the public, where individuals align their views on vaccines with their political identities rather than scientific evidence. Media outlets, too, contribute by amplifying these divides, often prioritizing sensationalism over nuanced reporting, further entrenching polarized viewpoints.
Social media platforms have also played a significant role in deepening vaccine polarization. Algorithms designed to maximize engagement often prioritize controversial or emotionally charged content, creating echo chambers where users are exposed primarily to information that reinforces their existing beliefs. Misinformation and conspiracy theories about vaccines spread rapidly in these environments, particularly among groups already skeptical of government or scientific institutions. When such misinformation aligns with political narratives—for instance, portraying vaccines as a tool of control by a particular party—it gains traction and becomes a partisan issue. This dynamic makes it increasingly difficult to bridge the gap between opposing sides, as facts and evidence are often dismissed in favor of ideological loyalty.
The consequences of this polarization are profound, particularly for public health. When vaccines become partisan, vaccination rates can decline in communities where skepticism is fueled by political rhetoric. This not only endangers individuals but also undermines herd immunity, leaving populations vulnerable to outbreaks. For example, counties in the U.S. with higher proportions of Republican voters saw lower COVID-19 vaccination rates, reflecting how political polarization directly impacted public health outcomes. Moreover, the politicization of vaccines erodes trust in scientific institutions, making it harder to address future health crises that require widespread cooperation.
To address this issue, it is crucial to depoliticize vaccine debates and restore trust in science and public health institutions. This requires bipartisan efforts to communicate the benefits of vaccines in a non-partisan manner, emphasizing their role in protecting communities rather than advancing political agendas. Public health officials and scientists must also engage with skeptical communities, addressing their concerns transparently and empathetically. Additionally, media and social platforms need to take responsibility for curbing the spread of misinformation and promoting evidence-based discourse. By refocusing the conversation on shared values like health and safety, it may be possible to reduce polarization and rebuild consensus around the importance of vaccines.
Do Political Parties Endorse Candidates During Primary Election Seasons?
You may want to see also

Corporate influence on vaccine development raises public suspicion
The role of corporations in vaccine development has become a significant source of public suspicion, fueling the politicization of vaccines. Pharmaceutical companies, driven by profit motives, often invest heavily in research, development, and marketing of vaccines. While their expertise and resources are crucial for producing life-saving vaccines, their financial incentives can create conflicts of interest. For instance, corporations may prioritize vaccines with higher profit margins over those addressing urgent public health needs in low-income regions. This perceived prioritization of profit over public health erodes trust, as people question whether vaccine development is guided by corporate greed rather than genuine concern for global well-being.
Corporate influence extends beyond research and development to regulatory processes and public policy. Pharmaceutical companies lobby governments and health organizations to expedite vaccine approvals, sometimes raising concerns about shortcuts in safety and efficacy testing. High-profile cases of rushed approvals or side effects, such as the AstraZeneca vaccine’s rare blood clotting incidents, amplify public skepticism. Additionally, corporations fund political campaigns and advocacy groups, further blurring the lines between public health interests and corporate agendas. This interplay between industry and politics makes vaccine policies appear biased, fostering suspicion among those who view such collaborations as corrupt or self-serving.
The pricing and distribution of vaccines also highlight corporate influence and deepen public mistrust. During the COVID-19 pandemic, for example, pharmaceutical giants like Pfizer and Moderna faced criticism for high vaccine prices and inequitable distribution, particularly in developing countries. While corporations defended their pricing as necessary to recoup research costs, the public perceived it as profiteering during a global crisis. Intellectual property rights, such as patents, further restrict access, as corporations resist calls for vaccine technology sharing. This exclusivity reinforces the narrative that corporate interests trump global health equity, making vaccines a symbol of systemic inequality and corporate dominance.
Transparency, or the lack thereof, in corporate practices exacerbates suspicion. Pharmaceutical companies often cite proprietary information to withhold data on vaccine trials, manufacturing processes, or pricing structures. While trade secrets are a legitimate concern, the opacity fuels conspiracy theories and mistrust. For instance, rumors about hidden ingredients or long-term side effects gain traction when corporations fail to communicate openly. Public health experts argue that greater transparency could rebuild trust, but corporations are often reluctant to disclose information that might impact their competitive edge or expose them to legal risks.
Finally, corporate marketing and messaging around vaccines contribute to public suspicion. Aggressive advertising campaigns, partnerships with influencers, and sponsored content can make vaccine promotion feel like a sales pitch rather than a public health initiative. When corporations frame vaccination as a personal responsibility or a moral duty, it can alienate those who view it as a collective societal issue. This commercialization of health decisions reinforces the perception that corporations manipulate public opinion for financial gain, further politicizing vaccines and deepening divisions between pro-vaccine and anti-vaccine groups.
In summary, corporate influence on vaccine development, from research to distribution, raises public suspicion by creating conflicts of interest, prioritizing profit, and fostering inequity. The interplay between industry and politics, coupled with a lack of transparency and aggressive marketing, fuels mistrust and politicizes vaccines. Addressing these concerns requires balancing corporate involvement with robust regulatory oversight, equitable distribution, and transparent communication to restore public confidence in vaccines as a vital public health tool.
BC Political Donations: Can Corporations Legally Support Parties?
You may want to see also
Explore related products

Mandatory vaccine policies clash with individual freedom arguments
The debate surrounding mandatory vaccine policies often centers on the perceived clash between public health imperatives and individual freedoms. Proponents of mandatory vaccination argue that it is a necessary measure to achieve herd immunity, protect vulnerable populations, and prevent the spread of infectious diseases. However, opponents contend that such policies infringe upon personal autonomy, forcing individuals to make medical decisions they may not consent to. This tension highlights the broader political divide between collective welfare and individual rights, making vaccines a contentious issue in policy-making.
One of the primary arguments against mandatory vaccine policies is rooted in the principle of bodily autonomy. Critics assert that individuals have the right to decide what substances are introduced into their bodies, regardless of societal benefits. This perspective often aligns with libertarian or conservative ideologies that prioritize personal freedom over government intervention. Mandatory vaccination, in this view, is seen as an overreach of state power, undermining the trust between citizens and their government. The historical context of medical experimentation on marginalized groups further fuels skepticism, as some communities view such policies as a continuation of systemic coercion.
Another layer of the individual freedom argument involves concerns about informed consent and medical choice. Opponents of mandates argue that vaccination decisions should be made after careful consideration of personal health risks, potential side effects, and alternative preventive measures. They claim that mandatory policies disregard individual differences in health status, allergies, or religious beliefs, effectively stripping people of their right to make informed choices. This stance is often amplified by anti-vaccine movements, which, while not representative of the majority, have gained traction by framing the issue as a fight against authoritarianism.
The political nature of this debate is further exacerbated by the role of misinformation and distrust in institutions. In an era of polarized media and declining faith in scientific authorities, mandatory vaccine policies are sometimes portrayed as tools of control rather than public health measures. This narrative resonates with those who feel marginalized by mainstream politics, creating a fertile ground for resistance. As a result, what begins as a medical and scientific issue quickly becomes a political battleground, where individual freedoms are pitted against the greater good.
Ultimately, the clash between mandatory vaccine policies and individual freedom arguments reflects deeper societal values and ideological differences. Resolving this conflict requires balancing the need for collective health protection with respect for personal autonomy. Policymakers must navigate this delicate terrain by fostering transparency, addressing legitimate concerns, and implementing measures that minimize coercion while maximizing public safety. Until this balance is achieved, vaccines will remain a politically charged issue, symbolizing the ongoing struggle between individual rights and communal responsibilities.
Political Parties: Uniting or Dividing National Opinions?
You may want to see also

Global vaccine distribution inequity sparks political tensions
The inequitable distribution of vaccines across the globe has become a significant source of political tension, exacerbating existing divides between wealthy and low-income nations. During the COVID-19 pandemic, high-income countries hoarded vaccine doses, securing multiple times the quantities needed for their populations, while many low-income countries struggled to access even a fraction of the required doses. This disparity was not merely a logistical issue but a political one, as it highlighted the power dynamics in global health governance. Wealthy nations prioritized their own populations, often through advance purchase agreements with pharmaceutical companies, leaving little room for equitable global distribution. This vaccine nationalism fueled resentment and mistrust among less affluent nations, which felt abandoned by the international community during a global crisis.
The role of international organizations, such as the World Health Organization (WHO) and the COVAX initiative, further underscores the political nature of vaccine distribution. COVAX was established to ensure equitable access to vaccines, but it faced significant challenges due to insufficient funding, vaccine shortages, and the reluctance of wealthy nations to share doses. This failure exposed the limitations of global cooperation and the dominance of national interests over collective well-being. Low- and middle-income countries accused wealthier nations of undermining multilateral efforts, deepening political fissures and eroding trust in global institutions. The inequity in vaccine distribution thus became a symbol of broader systemic inequalities in the global order.
Geopolitical rivalries have also played a critical role in shaping vaccine distribution and its political implications. During the pandemic, vaccines became tools of diplomatic influence, with countries like China, Russia, and India using vaccine exports to strengthen their geopolitical standing. For instance, China's "vaccine diplomacy" aimed to enhance its global image and counter criticism of its handling of the pandemic's early stages. However, this approach created tensions with Western nations, which viewed such efforts as a challenge to their own influence. The politicization of vaccines in this manner not only distracted from the urgent public health need but also deepened ideological divides, further complicating global cooperation.
The inequity in vaccine distribution has had long-term political consequences, particularly in terms of global solidarity and the perception of fairness. Many low-income countries feel that the international community failed them during a critical moment, reinforcing a narrative of exploitation and neglect. This sentiment has fueled anti-Western sentiments in some regions and strengthened calls for self-reliance in health security. Moreover, the prolonged lack of access to vaccines in poorer nations has allowed the virus to mutate and spread, prolonging the pandemic and affecting global economic recovery. This has led to accusations that wealthy nations' short-sighted policies have ultimately harmed everyone, including themselves, further politicizing the issue.
Addressing global vaccine inequity requires not only immediate solutions but also systemic reforms to prevent future crises. Proposals include waiving intellectual property rights for vaccines, increasing manufacturing capacity in low-income countries, and establishing more robust global health frameworks. However, these measures face political resistance, particularly from pharmaceutical companies and nations benefiting from the status quo. The debate over vaccine equity has thus become a battleground for competing visions of global governance, with profound implications for international relations. Until these issues are resolved, vaccine distribution will remain a politically charged topic, reflecting deeper inequalities and power imbalances in the world.
Do Third Party Votes Matter in Today's Political Landscape?
You may want to see also
Frequently asked questions
Vaccines often become political when they intersect with debates over individual rights, government authority, and public health policies. Political ideologies and mistrust in institutions can influence how people perceive vaccine mandates or recommendations.
In many countries, political parties may differ in their approach to vaccines based on their core values. For example, some parties emphasize personal freedom and oppose mandates, while others prioritize collective health and support vaccination campaigns.
Vaccine controversies often arise during elections because politicians may use them to appeal to specific voter bases or to criticize opponents. Public health issues can become politicized as a strategy to gain support or shift public focus.
Misinformation and disinformation about vaccines can fuel political divisions by creating fear and distrust. Political actors may amplify false claims to align with their agendas, further polarizing public opinion on vaccination.