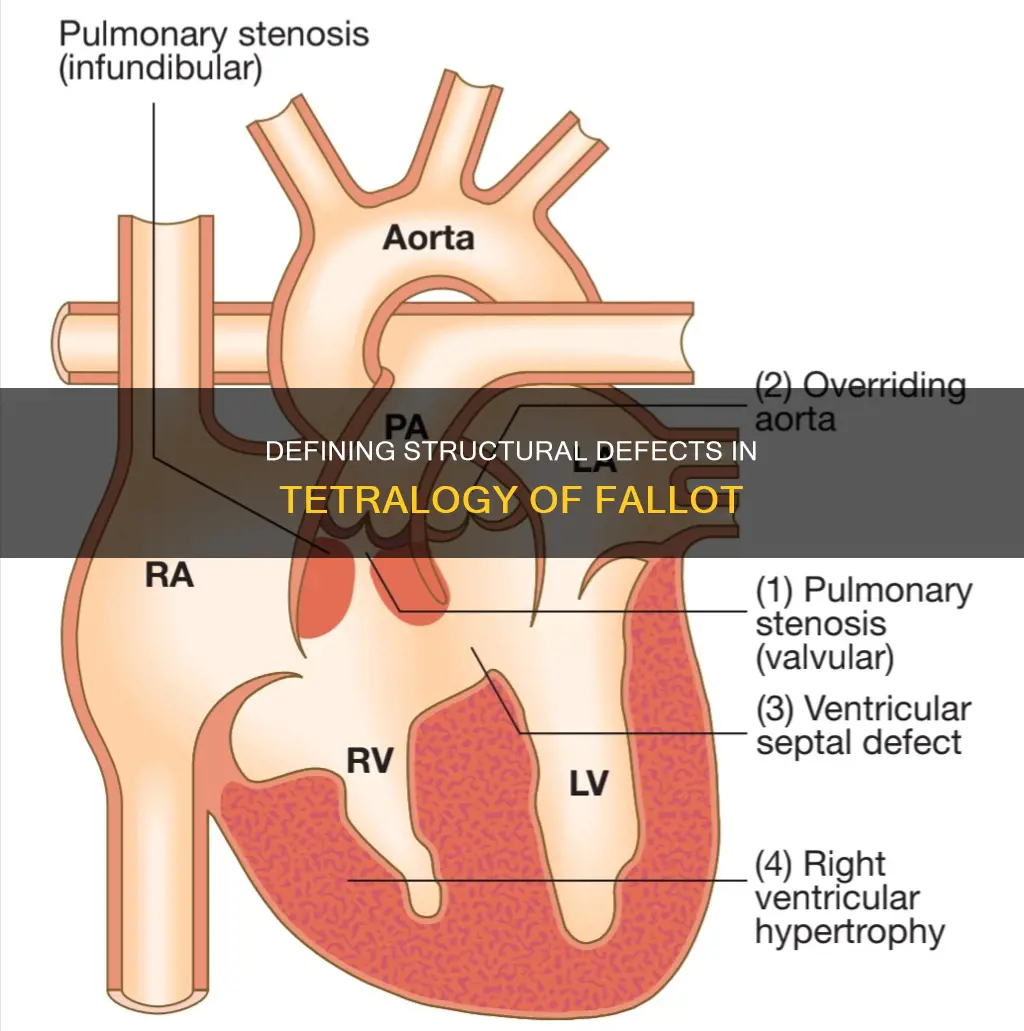
Tetralogy of Fallot is a congenital heart defect that affects the structure of the heart. It is characterised by four distinct abnormalities that alter the normal flow of blood through the heart, resulting in a mix of oxygenated and deoxygenated blood. These four structural defects are: a ventricular septal defect, pulmonary stenosis, an overriding aorta, and right ventricular hypertrophy. The combination of these defects leads to a range of symptoms, including bluish skin, difficulty breathing, and poor growth. The condition is named after French doctor Etienne-Louis Arthur Fallot, who provided a detailed description of the condition in the 19th century.
| Characteristics | Values |
|---|---|
| Ventricular septal defect (VSD) | A large hole in the wall that separates the ventricles (the lower chambers of the heart) |
| Pulmonary stenosis | Narrowing or obstruction of the pulmonary valve, which connects the right ventricle and the pulmonary artery |
| Overriding aorta | The aorta is positioned straddling the VSD, allowing oxygen-rich and oxygen-poor blood to mix as it is pumped to the body |
| Right ventricular hypertrophy | Thickening of the muscle wall of the right ventricle as a result of the muscle working harder to pump blood |
Explore related products
What You'll Learn

Ventricular septal defect (VSD)
VSD occurs when the muscular wall that separates the heart into left and right sides does not form fully during a baby's development in the womb, leaving one or more holes. The size of the hole, or holes, can vary, and there is often no clear cause for its occurrence. However, genetics and environmental factors may play a role. In some cases, VSD can occur later in life after a heart attack or certain heart procedures, but this is rare.
The hole caused by VSD allows oxygen-rich blood to flow back into the lungs instead of being pumped out to the rest of the body. This changes the normal direction of blood flow in the heart and lungs, increasing the amount of blood that flows through the lungs. As a result, the heart and lungs have to work harder to pump blood, which can lead to an increased risk of other complications over time if left untreated.
The symptoms of VSD depend on the size of the hole and the presence of other heart problems. Small VSDs may not cause any symptoms and can even close on their own without requiring treatment. However, medium or large VSDs may require surgery early in life to prevent complications. Larger holes can cause symptoms such as difficulty with growth and breathing, and if left untreated, can lead to serious complications like pulmonary hypertension and lung disease.
The US Constitution: Our Nation's Most Vital Document
You may want to see also

Narrowing of the pulmonary valve
Pulmonary stenosis is a condition in which the pulmonary valve is narrowed, restricting blood flow from the heart to the lungs. This narrowing can cause the right ventricle to pump at abnormally high pressures, leading to right ventricular hypertrophy. The obstruction in the right ventricular outflow tract (RVOTO) is a result of the narrowed pulmonary valve and is present in the majority of cases of TOF. The severity of RVOTO can vary, and it is this variation that largely determines the clinical presentation of TOF.
The pulmonary valve itself may be dysplastic and stenotic, while the pulmonary valve annulus is often hypoplastic. In the most severe form of TOF, the pulmonary valve is atretic, meaning it is completely closed and non-functional. This severe form of the anomaly occurs in approximately 15% of cases. In some instances, pulmonary atresia can develop over time, even if the patient did not initially present with this condition.
The narrowing of the pulmonary valve and RVOTO can cause a reduction in arterial oxygen saturation, resulting in cyanosis, where oxygen-poor blood appears blue in the skin and lips. This cyanosis can range from mild to severe, depending on the extent of the narrowing. In cases of severe RVOTO, prompt stabilisation is crucial to prevent profound cyanosis and rapid deterioration.
Treatment for TOF often involves surgical intervention to augment, or enlarge, the right ventricular outflow tract and pulmonary valve. This is achieved by cutting away obstructive muscle tissue and enlarging the outflow pathway with a patch. In some cases, a conduit (tube) may be sewn from the right ventricle to the bifurcation of the pulmonary arteries to ensure unobstructed blood flow.
Vital Documents: Proving Your Date of Birth Legally
You may want to see also

Overriding aorta
Tetralogy of Fallot (ToF) is a congenital heart defect characterised by a combination of four specific heart abnormalities. One of these is an overriding aorta, which is present in around 10% of babies with a heart abnormality at birth.
An overriding aorta is a defect where the aorta, which carries oxygen-rich blood to the body, is shifted slightly to the right and overrides both ventricles, instead of originating exclusively from the left ventricle. This results in the aorta receiving some blood from the right ventricle, causing oxygenated and deoxygenated blood to mix, reducing the amount of oxygen delivered to the tissues. This can be diagnosed by echocardiography, which provides detailed images of the heart, and is the primary tool for diagnosing ToF.
Babies born with ToF often appear cyanotic, or blue, due to the oxygen-poor blood being pumped out to the body, causing a reduction in arterial oxygen saturation. This cyanosis is more pronounced when there is a narrower outflow tract from the right ventricle, as this restricts blood flow to the lungs, lowering arterial oxygen levels.
Surgical repair of ToF has been performed since the 1950s, and is successful in most people. Surgery involves closure of the ventricular septal defect, allowing blood to flow normally from the left ventricle to the aorta. In some cases, a temporary shunt may be placed between the aorta and pulmonary artery to improve blood flow to the lungs until a complete repair can be performed.
Without treatment, the symptoms of ToF will worsen over time. However, more than 90% of babies who undergo surgery for ToF go on to live normal lives into their 70s and 80s.
Quoting the US Constitution: A Guide
You may want to see also
Explore related products

Right ventricular hypertrophy
Tetralogy of Fallot (TOF) is a congenital heart defect that includes four anatomical alterations. One of these is right ventricular hypertrophy, which is the thickening of the right pumping chamber (ventricle) wall. This is caused by the right part of the heart having to work harder, which is a consequence of the overriding aorta and pulmonary stenosis that are also present in TOF.
The right ventricle in TOF is subject to pressure overload and hypoxemia, followed by chronic volume overload due to pulmonary regurgitation after corrective surgery. This results in right ventricular dysfunction, which is a major determinant of outcomes in patients with complex congenital heart disease. The dysfunction can be described as a syndrome of dysfunctional characteristics affecting both contraction and filling.
The right ventricle in TOF has a unique phenotype with important distinctions from other types of heart failure. Combining insights from clinical and experimental physiology and myocardial (tissue) data has helped identify this phenotype. The characteristics of the right ventricle in TOF are the end result of several adaptation pathways of the cardiomyocytes, myocardial vasculature, and extracellular matrix.
Right ventricular dysfunction is also a common complication after surgery for TOF. The right ventricle is "stiff" from the previous hypertrophy, and an incision is made into the muscle of the ventricle, making it temporarily weaker. This dysfunction usually improves significantly in the days following surgery.
Overall, right ventricular hypertrophy is a critical component of TOF, and understanding its unique characteristics and adaptations is essential for effective management and treatment.
Citing the Constitution: MLA Clause Format
You may want to see also

Cyanosis
Tetralogy of Fallot is one of the most common cyanotic congenital heart defects, accounting for 5–10% of all congenital cardiac malformations. It is characterised by four key features: a ventricular septal defect (VSD), right ventricular outflow tract obstruction (RVOTO), an overriding aorta, and right ventricular hypertrophy (RVH).
The presence of these structural defects results in low oxygen levels in the blood, leading to a condition called cyanosis, characterised by a bluish or bluish-purple discolouration of the skin. Long-standing cyanosis can have significant consequences, including an increased production of red blood cells, which can clog the circulation and lead to long-term health issues.
The severity of cyanosis in Tetralogy of Fallot is determined by the degree of obstruction to pulmonary blood flow. The narrowing of the subpulmonary and pulmonary valves in this condition restricts blood flow to the lungs, resulting in reduced oxygenation of the blood. This obstruction can vary in degree and may be influenced by factors such as a stenotic pulmonary valve, a hypoplastic pulmonary valve annulus, or deviation of the infundibular septum.
In cases of significant cyanosis, early intervention is often required, sometimes within the first week of life. A common treatment is the creation of a shunt, which establishes a connection between the systemic and pulmonary circulations, facilitating oxygenated blood flow to the lungs. Fetal echocardiography can aid in prenatal diagnosis, allowing for prompt stabilisation and prevention of severe cyanosis in infants with Tetralogy of Fallot.
The management of cyanosis in Tetralogy of Fallot also includes preventing cyanotic spells, which can be life-threatening. Surgical correction is recommended to address the underlying structural defects and improve blood oxygenation. The surgery typically involves closing the VSD and widening the outflow to the lungs, and it carries a good prognosis when performed early.
The Executive Branch: Powers and Limits
You may want to see also