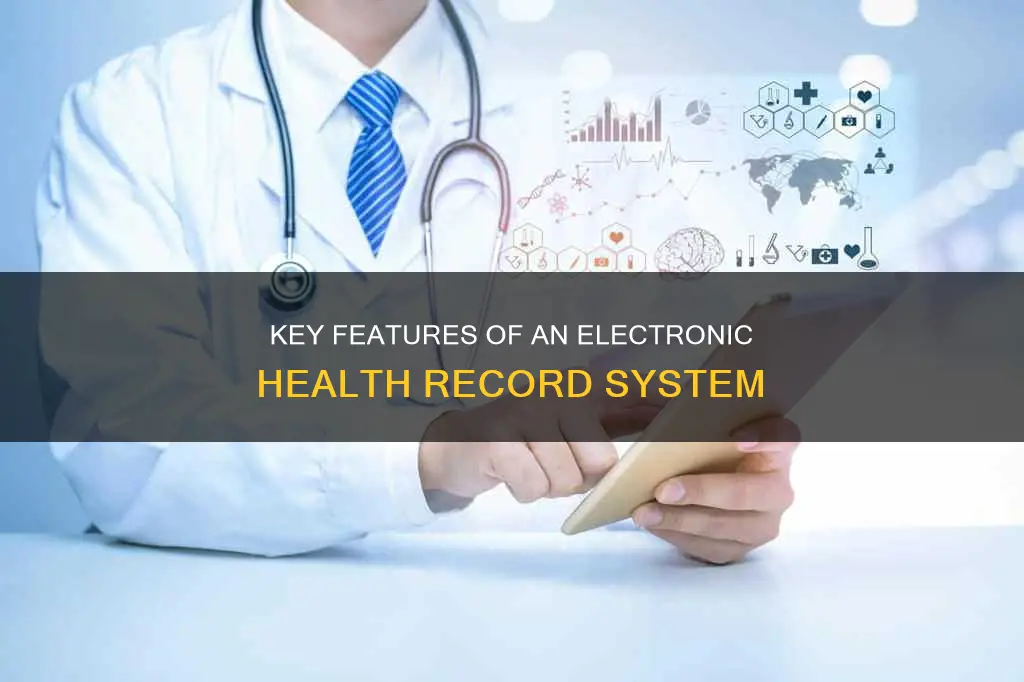
Electronic Health Records (EHRs) are digital versions of patients' medical histories, maintained by healthcare providers. They are designed to streamline clinician workflows and improve patient care by providing accurate, up-to-date, and complete information. EHRs can include demographics, progress notes, medications, vital signs, past medical history, laboratory data, and radiology reports. They facilitate information sharing between healthcare providers and patients, enhancing communication, efficiency, and safety. Additionally, EHRs can support evidence-based decision-making, quality management, and outcomes reporting. The implementation of EHRs is a step towards transforming healthcare and empowering patients and providers with accessible, coordinated health information. However, challenges related to standardization, security, and potential errors must be addressed to fully realize the benefits of EHR systems.
| Characteristics | Values |
|---|---|
| Definition | A compilation of software routines that provide all the features and functions required to help clinicians practice medicine |
| Other Names | Electronic patient record (EPR), electronic medical record (EMR), personal health record (PHR) |
| Data Included | Demographics, progress notes, problems, medications, vital signs, past medical history, immunizations, laboratory data, radiology reports, clinical observations, investigations, treatment data, legal permissions |
| Benefits | Improved patient care, better health outcomes, improved efficiency, reduced costs, improved safety, improved communication, improved patient interaction, improved convenience, better diagnosis, reduced medical errors |
| Functions | Data capture, order creation, information sharing, recording clinician findings, thoughts, and actions, storage of an accurate and complete copy of a patient’s health record |
| Record Standardization | OMOP Common Data Model, PCORNet Common Data Model, Virtual Data Warehouse |
| Length of Storage | Depends on national and state regulations; typically between 20 and 100 years |
Explore related products
$50.98 $72.99
$17.81 $72.99
What You'll Learn

Data capture
An Electronic Health Record (EHR) is an electronic version of a patient's medical history, maintained by the provider, that may include all the key administrative clinical data relevant to the patient's care. EHRs are designed to improve patient care, safety, effectiveness, communication, efficiency, and equity. They can also encourage healthier lifestyles in the wider population.
The integration of real-time data (RTD) in EHRs is transforming healthcare. RTD can be captured through various mechanisms, including database triggers, reverse proxies, and subscriptions. For example, a subscription resource with specific criteria can be created to generate notifications when certain conditions are met. This allows for efficient and timely updates to be sent to recipients in real-time.
However, challenges exist in capturing RTD, and the design and implementation of systems for this purpose require careful consideration. Database triggers, for instance, need to be designed carefully to avoid performance bottlenecks and potential issues, especially in high-velocity RTD environments. Additionally, the choice of the database system and its support for real-time processing can impact the effectiveness of using triggers.
Furthermore, the quality of data in EHRs is important. Evaluating data quality, completeness, and accuracy should be an ongoing process. EHRs often contain unstructured data, such as progress notes, which can be challenging for automating EHR-based registries. Standardization of data is crucial, and organizations like the International Organization for Standardization (ISO) have adopted standards for EHR systems.
Checks and Balances: Indirect Elections' Role
You may want to see also

Information sharing
EHRs facilitate the systematic integration of patient data from different specialties, creating a shared and comprehensive health record. This enables simultaneous access to patient information, independent of time and place, fostering mutual understanding and coordination among healthcare professionals. The ability to access patient records quickly improves the coordination and efficiency of care, reducing the duplication of tests and treatments.
The sharing of patient information electronically also enhances communication between healthcare providers and patients. Patients can access their medical records and share them securely with other clinicians, improving interaction and enabling better clinical decision-making. This empowers patients to monitor their medical records and receive notifications for any unauthorized access, addressing privacy concerns.
In addition, EHRs enable the standardization and harmonization of health data from multiple institutions, allowing for a unified view of patient information. This interoperability improves the sharing of patient data across healthcare organizations and IT systems, even across borders. However, this increased sharing of sensitive information has raised concerns about data privacy and security, with the potential for privacy breaches.
To address these concerns, countries like the United States and the EU have implemented mandatory medical data breach notifications. Additionally, laws such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States and the Personal Information Protection and Electronic Documents Act (PIPEDA) in Canada have been enacted to safeguard patient information and protect their privacy rights. These measures aim to balance the benefits of information sharing in EHRs with the need to secure sensitive healthcare data.
California Break Room Requirements: What You Need to Know
You may want to see also

Recording clinician notes
An Electronic Health Record (EHR) is an electronic version of a patient's medical history, which is maintained by the provider over time. It may include all the key administrative clinical data relevant to a patient's care, such as demographics, progress notes, problems, medications, and vital signs. Recording clinician notes is an essential aspect of EHRs, providing a detailed account of patient interactions.
Clinical notes are a summary of the interactions between patients and healthcare providers. They capture the reasons for a diagnosis, recommended treatments, and any ruled-out conditions. These notes are intended for healthcare professionals, but patients can also benefit from reviewing them to better understand their care. Structured entry systems are used to capture data in real time, producing information that can facilitate automated reminders and alerts, as well as support other clinical tasks.
There are various methods for generating clinical notes in EHR systems. One simple method is "Type New Document", which provides a blank text box for clinicians to type their notes. This tool is easily accessible and allows for plain-text formatting, but it does not offer templates or data reuse capabilities. Another method is dictation, where a healthcare provider speaks into a recording device, and a transcriptionist produces the clinical note. Transcription can be done by a human, a specialised computer program, or a combination of both.
The Vanderbilt experience, as described in one source, highlights the importance of selecting a documentation method based on clinical workflow, note content standards, and usability considerations. A "one-size-fits-all" approach may not work due to the varying needs of different healthcare providers and specialties. For example, certain specialties may require more structured and standardised documentation, while others may prioritise flexibility and comfort with the system.
Overall, recording clinician notes in EHRs is a complex process that requires careful consideration of the documentation methods used. It plays a crucial role in improving patient care, facilitating better decision-making, and strengthening the relationship between patients and clinicians.
Core Principles of a Constitutional Democracy
You may want to see also
Explore related products

Patient data storage
An Electronic Health Record (EHR) is a digital version of a patient's medical history. EHRs are used to collect and store patients' medical information, including medical history, diagnoses, treatment plans, lab results, demographics, progress notes, medications, vital signs, immunizations, and radiology reports. This information is captured and stored electronically, making it accessible to authorized users within and outside hospitals.
EHRs provide a holistic view of a patient's health, including clinical data and other relevant information. They are maintained by healthcare providers over time and are designed to be visit-centred and transactional. The data in EHRs is securely stored and accessible only to authorized healthcare professionals and patients. This ensures compliance with privacy regulations, such as HIPAA, and protects sensitive patient information.
The length of time EHR data is stored depends on national and state regulations, with typical preservation times ranging from 20 to 100 years. To ensure data security and accessibility, cloud-based EHR storage is often preferred over in-house storage. Cloud-based systems offer advanced data encryption and protection, even in the event of a security breach.
EHRs improve patient care by providing accurate and up-to-date information, enabling quick access to patient records, facilitating secure information sharing, and enhancing communication between patients and providers. Additionally, EHRs reduce costs by decreasing paperwork, improving safety, and reducing duplicate testing.
Overall, EHRs offer a comprehensive and accessible means of storing patient data, contributing to improved patient care and health outcomes.
Voltaire's Admiration for English Constitution Explained
You may want to see also

Administrative processes
EHRs automate access to information, enabling quick access to patient records, which improves efficiency and coordination of care. They replace paper or handwritten medical records, which can be incomplete, illegible, or misplaced. This digitalisation improves data security and integrity, reducing the chances of unauthorised access.
EHRs also support administrative processes by facilitating the sharing of patient information between healthcare organisations and IT systems. This improves communication and coordination between different providers, especially when a patient receives care from multiple facilities. The ability to securely exchange health information electronically is a significant advantage, improving patient care and safety.
Additionally, EHRs enhance data collection and evaluation, providing opportunities for the implementation of genomic medicine and practices. They offer immediate access to comprehensive patient data, including demographics, progress notes, medications, vital signs, and past medical history. This supports administrative processes by enabling more informed decision-making and improved patient management.
EHR systems also benefit administrative processes by reducing costs. The use of EHRs decreases paperwork, reduces duplication of testing, and improves efficiency, resulting in lower overall healthcare expenses.
The Chief Justice's Constitution: John Marshall's Vision
You may want to see also
Frequently asked questions
An EHR is an electronic version of a patient's medical history, maintained by the provider and including administrative clinical data such as demographics, progress notes, medications, and laboratory data.
EHRs improve patient care by streamlining clinician workflow, improving coordination between healthcare providers, and providing accurate and up-to-date patient information. They also reduce costs by decreasing paperwork and duplication of tests.
The terms EHR, EMR, and EPR are often used interchangeably, but there are subtle differences. An EHR is a longitudinal collection of electronic health information from multiple providers, while an EMR is a digital version of the paper records created by a specific practice or hospital. A PHR is an electronic application for recording medical data that is controlled by the patient.
EHRs are vulnerable to unauthorized access and may pose threats to patient privacy. They can also be costly to implement and maintain, and may lack innovation and operational flexibility.

















![Norton 360 Deluxe 2025, Antivirus software for 3 Devices with Auto-Renewal – Includes Advanced AI Scam Protection, VPN, Dark Web Monitoring & PC Cloud Backup [Download]](https://m.media-amazon.com/images/I/719bgx+IiYL._AC_UY218_.jpg)