Deep vein thrombosis (DVT) is a common and potentially fatal disease that involves the formation of a blood clot in a deep vein, most commonly in the legs or pelvis. It can also occur in the arms and the mesenteric and cerebral veins. DVT is caused by sluggish blood flow due to injury or immobilization, and it can lead to life-threatening complications such as pulmonary embolism (PE) when blood clots travel to the lungs. The condition is diagnosed through ultrasound and treated with anticoagulants or blood-thinning medications. Lifestyle changes, such as regular exercise, weight management, and avoiding smoking, can help prevent DVT.
| Characteristics | Values |
|---|---|
| Veins Affected | Deep veins, usually in the leg, but can occur in the arms and the mesenteric and cerebral veins |
| Types | Isolated calf vein (distal), femoropopliteal, and iliofemoral thrombosis |
| Symptoms | Pain, swelling, redness, enlarged veins, throbbing pain, skin discolouration, leg ulcers, shortness of breath, chest pain, rapid breathing, rapid pulse, feeling faint, coughing up blood |
| Risk Factors | History of DVT, limited blood flow, immobilization, obesity, older than 40, pregnancy, autoimmune disease, smoking, varicose veins, birth control pills, central venous catheter, pacemaker, COVID-19 |
| Treatment | Anticoagulants, blood-thinning medicine, ultrasound surveillance, compression stockings |
Explore related products
What You'll Learn
- Risk factors: Obesity, pregnancy, age, surgery, critical care, dehydration, and cancer
- Symptoms: Pain, swelling, redness, enlarged veins, or no symptoms at all
- Prevention: Move legs, avoid crossing legs, exercise, and manage weight
- Diagnosis: Ultrasound, blood tests, and imaging tests
- Treatment: Anticoagulants, blood-thinning medicine, and compression stockings

Risk factors: Obesity, pregnancy, age, surgery, critical care, dehydration, and cancer
Obesity is a risk factor for deep vein thrombosis (DVT). Excess body weight increases pressure in the veins in the pelvis and legs. Regular exercise lowers the risk of blood clots. As a general goal, aim for at least 30 minutes of moderate physical activity every day.
Pregnancy is also a risk factor for DVT. It increases pressure in the veins in the pelvis and legs. The risk of DVT is up to five times higher in pregnant women. Pelvic vein thrombosis, which is uncommon outside of pregnancy, accounts for 6–11% of DVT during pregnancy. During normal pregnancy, a hypercoagulable state is initiated, which is the most important risk factor contributing to thrombosis during pregnancy.
Age is another factor that affects the likelihood of experiencing DVT. While DVT can occur at any age, being older than 60 increases the risk.
DVT can also be caused by surgery, particularly if it directly damages a vein. In addition, being on bed rest after surgery can increase the risk of blood clots.
Dehydration is a known independent risk factor for the development of DVT. However, there is possibly insufficient evidence to form a strong association.
Cancer is also a risk factor for DVT. Certain cancers and cancer treatments increase substances in the blood that cause it to clot.
Women's Impact on the Declaration and Constitution
You may want to see also

Symptoms: Pain, swelling, redness, enlarged veins, or no symptoms at all
Deep vein thrombosis (DVT) occurs when a blood clot (thrombus) forms in one or more of the deep veins in the body, usually in the legs. The condition can be serious because blood clots in the veins can break loose, travel through the bloodstream, and get stuck in the lungs, blocking blood flow and leading to a pulmonary embolism (PE) – a life-threatening complication.
DVT symptoms vary with the anatomic distribution, extent, and degree of occlusion of the thrombus. Symptoms may range from absence to massive swelling and cyanosis with impending venous gangrene. Symptoms tend to be more severe as thrombosis extends more proximally. However, up to 50% of patients with acute DVT may lack specific signs or symptoms.
The most common symptoms of DVT are pain and swelling. Pain may be throbbing and is usually in the calf or thigh when walking or standing. It may worsen when bending the foot upwards. The affected area may also feel warm and tender. Red or darkened skin around the painful area can also be a symptom, though this may be difficult to see depending on skin tone.
Other symptoms of DVT include enlarged veins, increased pigmentation or skin discolouration, and leg ulcers known as venous stasis ulcers. However, in some cases, there may be no noticeable symptoms.
Founders' Political Parties: A Dangerous Necessity
You may want to see also

Prevention: Move legs, avoid crossing legs, exercise, and manage weight
Deep vein thrombosis (DVT) occurs when a thrombus (blood clot) develops in the deep veins of the body, often in the lower leg, thigh, or pelvis. While DVT itself is not life-threatening, the blood clots can break free, travel through the bloodstream, and become lodged in the lungs, resulting in a pulmonary embolism (PE), a life-threatening complication. To prevent DVT and its serious consequences, it is crucial to take proactive measures such as moving your legs, avoiding crossing your legs, exercising, and managing your weight.
Move Legs and Avoid Crossing Legs
Prolonged immobility increases the risk of developing DVT. Sitting for extended periods, whether during travel or after surgery, can lead to sluggish blood flow in the legs, promoting the formation of blood clots. Therefore, it is essential to move your legs frequently and avoid crossing your legs while seated. When travelling, take breaks to stretch and walk around. If you're on a plane, stand up and walk occasionally. If driving, stop every hour to walk and stretch your legs. If you're on bed rest, perform lower leg exercises, such as raising and lowering your heels or toes while keeping the rest of your foot on the floor.
Exercise
Exercise is a powerful tool in the prevention of DVT. It improves blood flow and helps prevent the formation of blood clots. Aim for at least 30 minutes of moderate physical activity daily. Walking exercises, in particular, are safe and effective for those with acute DVT and may even improve acute symptoms. Additionally, exercise training can improve calf muscle strength and pump function, further enhancing blood flow and reducing the risk of DVT.
Manage Weight
Obesity is a significant risk factor for DVT. Maintaining a healthy weight through regular exercise and a balanced diet can lower the likelihood of developing DVT. If you are overweight, increasing your physical activity beyond 30 minutes a day or adjusting your dietary habits may be necessary to achieve and sustain a healthy weight.
Violent Crime Charges in Pennsylvania: What You Need to Know
You may want to see also
Explore related products

Diagnosis: Ultrasound, blood tests, and imaging tests
Deep vein thrombosis (DVT) occurs when a thrombus (blood clot) develops in the deep veins of the body, usually in the lower leg, thigh, or pelvis. It can also occur in other parts of the body, including the arm, brain, intestines, liver, or kidney. While DVT itself is typically not life-threatening, the blood clots can break free and travel to the lungs, resulting in a pulmonary embolism, which can be fatal. Therefore, prompt diagnosis and treatment are crucial.
Ultrasound, blood tests, and imaging tests play a pivotal role in diagnosing DVT and ruling out other conditions. Let's delve into each of these diagnostic modalities:
Ultrasound:
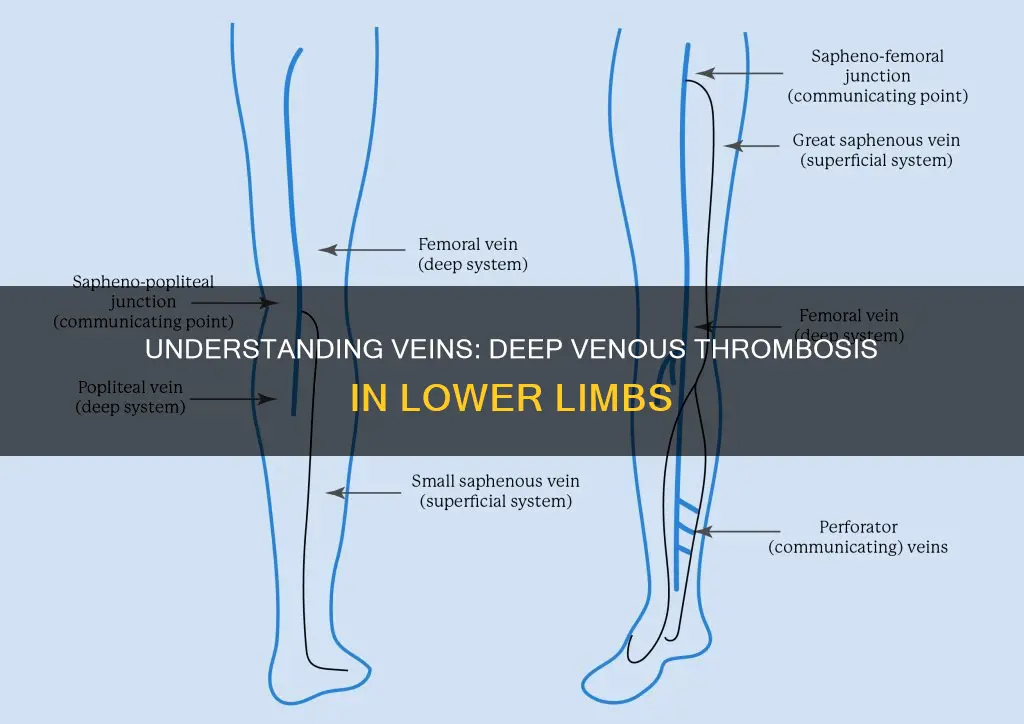
Ultrasound, particularly duplex venous ultrasound, is the most common test for diagnosing DVT. This non-invasive and widely available technique utilizes sound waves to visualize the deep veins and detect the presence of blood clots. The iliac vein, common femoral vein, deep femoral vein, femoral vein, popliteal vein, and their tributaries are well-visualized on ultrasound scans. The exam may include maneuvers such as the Valsalva and augmentation maneuvers to assess for venous insufficiency. Ultrasound is highly sensitive and specific for DVT, making it an excellent initial investigation. However, in certain cases, such as suspected thrombus in the upper extremities, additional imaging techniques like venography or magnetic resonance angiography (MRA) may be necessary.
Blood Tests:
Blood tests are crucial in the management of DVT, especially when anticoagulant or "blood thinner" medications are prescribed. These medications prevent clots from growing and new clots from forming. Commonly, blood tests are used to monitor the levels of anticoagulants in the body, such as warfarin (Jantoven), and to assess how well the blood is clotting. Additionally, blood tests can identify underlying conditions or risk factors that may contribute to DVT, such as autoimmune diseases or coagulation disorders.
Imaging Tests:
In addition to ultrasound, other imaging tests can aid in the diagnosis of DVT and its complications. Magnetic resonance angiography (MRA) is highly accurate for visualizing central thoracic veins and detecting thrombi. Computed tomography (CT) scan venography is particularly useful for detecting clots in the proximal lower limb veins, such as the iliac veins and inferior vena cava. These imaging modalities may involve the injection of contrast media, so patients with iodine allergies may require alternative imaging approaches or USG (ultrasound).
Understanding Child Abandonment Laws in Arizona
You may want to see also

Treatment: Anticoagulants, blood-thinning medicine, and compression stockings
Deep vein thrombosis (DVT) is a blood clot that forms within the deep veins, most commonly in the legs or pelvis, but it can also occur in the arms and the mesenteric and cerebral veins. It is a common venous thromboembolic (VTE) disorder with an incidence rate of 1.6 per 1,000 annually. Each year, approximately 1 to 3 in every 1,000 adults develop DVT or pulmonary embolism in the United States.
DVT can be dangerous as blood clots can travel to the lungs, resulting in a pulmonary embolism (PE), a life-threatening complication. The warning signs and symptoms of PE include sudden shortness of breath, chest pain while breathing in or coughing, rapid breathing, rapid pulse, feeling faint or fainting, and coughing up blood.
If you suspect you have DVT, it is important to seek medical help as soon as possible. Treatment for DVT aims to prevent the clot from breaking off and moving to the lungs, reducing the risk of another blood clot, and preventing long-term complications. This typically involves the use of anticoagulants, also known as blood-thinning medicines.
Anticoagulants:
Anticoagulants are the standard treatment for DVT and help prevent clots from growing larger or moving to other parts of the body. They do not dissolve existing clots but work by making it harder for the blood to clot. It is important to take anticoagulants exactly as prescribed by your healthcare provider and to not stop or start taking any other medications without consulting your provider.
Blood-thinning medicine:
Blood-thinning medicines, such as anticoagulants, are used to treat DVT and prevent blood clots from forming or growing larger. These medicines are typically started after patients are checked to ensure they are not at risk of excessive bleeding. Treatment duration and dosage may vary depending on the location of the DVT and the patient's risk of recurrence. For example, patients with isolated distal DVT at a high risk of VTE recurrence may receive a longer or higher-dose course of anticoagulation, while those at low risk may receive a shorter course or lower doses.
Compression stockings:
Compression stockings, also known as knee-high elastic socks, are another treatment option for DVT. They help improve blood circulation and can be worn during hospital stays and after discharge to lower the chances of developing DVT. They are often recommended for individuals at higher risk of DVT, such as those undergoing surgery or who are immobile.
Pennsylvania Work Drug Tests: What You Need to Know
You may want to see also
Frequently asked questions
Deep vein thrombosis (DVT) occurs when a thrombus (blood clot) develops in veins deep in the body. This is usually in the lower limb venous system, with clot formation often originating in a deep calf vein and growing in the direction of venous flow, towards the heart.
Symptoms of DVT include throbbing pain in one leg, usually in the calf or thigh, when walking or standing up. Other symptoms include swelling, redness, and enlarged veins in the affected area. However, some DVTs may not show any symptoms.
DVT in the lower extremities can affect the popliteal vein (behind the knee), femoral vein (of the thigh), and iliac veins of the pelvis. Extensive lower-extremity DVT can even reach the inferior vena cava in the abdomen.