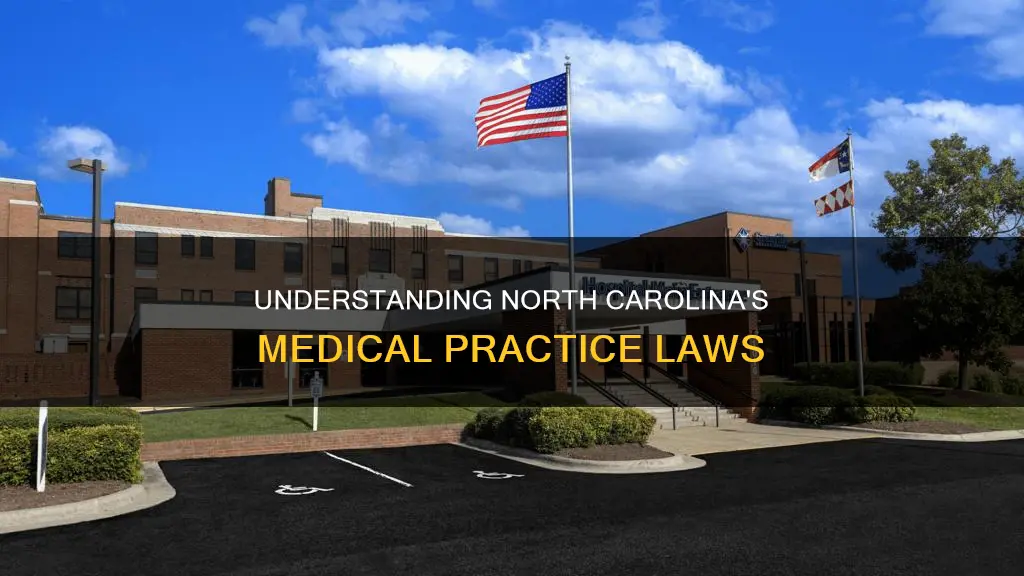
The practice of medicine in North Carolina is governed by Chapter 90 of the NC General Statute on medicine and allied health occupations. This chapter defines the practice of medicine and surgery and outlines the requirements for businesses practicing medicine in the state. It also establishes the North Carolina Medical Society, which is a body of regularly graduated physicians known as the North Carolina Medical Board. This board is responsible for overseeing and enforcing the practice of medicine in the state, including investigating and sanctioning licensees for violations. The board has recently published guidance on the corporate practice of medicine, addressing concerns regarding unlawful straw practices and the supervision of non-licensed entities by licensed physicians.
| Characteristics | Values |
|---|---|
| Administration of lethal substances | Does not constitute the practice of medicine or surgery |
| Advertising | Authorized to practice medicine in North Carolina |
| Prescribing drugs | Authorized to practice medicine in North Carolina |
| Preventing, diagnosing, correcting, prescribing, administering or treating any disease, illness, pain, wound, fracture, infirmity, defect, or abnormal physical or mental condition | Authorized to practice medicine in North Carolina |
| Performing any surgical procedure | Authorized to practice medicine in North Carolina |
| Businesses practicing medicine | Must be owned entirely by persons holding active North Carolina licenses |
| Hospitals and health maintenance organizations | Exempt from the above rule |
| Non-profit hospitals | Allowed to promulgate rules fixing the standards of those who may practice therein |
| Licensees providing medical services to businesses engaged in the corporate practice of medicine | May be subject to disciplinary action by the Board |
| Licensee's role | Whether a licensee is an employee or independent contractor is not determinative of whether they are aiding and abetting the corporate practice of medicine |
| Physician supervision | If a physician supervises a PA or NP employed by a non-licensed entity, they are implicated in potentially unlawful medical care |
| Licensee's health | If significantly impaired by alcohol, drug addiction or mental illness, the licensee shall be referred to the North Carolina Physicians Health Program |
| License status | A license can become inactive upon a licensee's request, failure to register annually, voluntary surrender, or based on any disciplinary order issued by the Board |
Explore related products
What You'll Learn

Advertising medical services
In North Carolina, advertising medical services is a practice that is governed by a set of rules and guidelines. The Medical Practice Act (MPA), which is Chapter 90 of the NC General Statute on medicine and allied health occupations, outlines the parameters within which medical professionals must operate when promoting their services.
According to the MPA, advertising medical services in North Carolina involves any act of promoting or representing oneself as authorized to practice medicine within the state. This includes advertising through various mediums, such as business letterheads, envelopes, and cards, which are all considered forms of publicity. Medical practitioners must ensure that their advertising and publicity materials do not create unjustified medical expectations or make deceptive claims. Statements implying exclusive skills or remedies are discouraged, as are claims of curing or successfully treating a high number of patients with a specific condition, as these can be misleading.
When using patient photographs in advertising, it is important to use only images of the licensee's own patients and to showcase realistic outcomes. Licensees are also responsible for updating their advertising content if changes in circumstances render it inaccurate or misleading. This includes ensuring that any patient notifications or informed consent procedures are included in direct advertising to the public. Additionally, with the advent of the internet, it is challenging for licensees to control all information about themselves in the public domain, so caution is advised.
The use of the term "board certified" is significant in North Carolina, as it signifies a physician's skill and training. To avoid deceptive advertising regarding board certification, physicians are expected to adhere to specific guidelines. Furthermore, when it comes to telehealth services, North Carolina has regulations in place to maintain the standard of care, including requirements for online prescribing, establishing the practitioner-patient relationship, patient identification, and maintaining medical records.
It is important to note that businesses practicing medicine in North Carolina are generally required to be fully owned by individuals with active North Carolina licenses. Non-profit hospitals and their medical practices are exempt from this rule.
Founding Fathers' Intent: Rewrite or Keep the Constitution?
You may want to see also

Prescribing drugs
The North Carolina Controlled Substances Act (NCCSA) is a key piece of legislation governing the prescribing of controlled drugs. The Act requires facilities that stock controlled substances to be registered and compliant with the NCCSA. It also outlines the process for administering psychotropic drugs, including the requirement for patient education and informed consent.
Prescribers of controlled substances must be aware of and comply with federal and state laws, including the evolving standards for e-prescribing. Pre-signing prescriptions is unacceptable, and each medication prescribed must be documented in the patient's medical record. A licensee-patient relationship, based on a medical history, physical examination, and prevailing standards of care, is required before prescribing.
Advanced Practice Registered Nurses (APRNs) with prescriptive authority must complete continuing education requirements, including training on controlled substance prescribing practices and the signs of abuse or misuse. APRNs must also register with the North Carolina Department of Health and Human Services Drug Control Unit and meet waiver requirements to prescribe Medically Assisted Therapy.
Nurse Practitioners (NPs) have more limited prescribing authority and must obtain a DEA number to prescribe controlled substances. NPs can only dispense drugs under the supervision of a licensed consulting pharmacist from a facility with a valid pharmacy permit. They must also obtain approval from the NC Board of Pharmacy to dispense drugs and devices.
Overall, the prescribing of drugs in North Carolina is a complex and highly regulated area, with specific requirements varying based on the type of medication and the role of the healthcare provider.
Executive Power: Is the Balance of Powers Unbalanced?
You may want to see also

Diagnosing and treating diseases
The North Carolina Medical Board (NCMB) defines the practice of medicine in Chapter 90 of the NC General Statute on medicine and allied health occupations. According to the statute, the practice of medicine includes:
> Advertising, holding out to the public, or representing in any manner that the individual is authorized to practice medicine in this State. Offering or undertaking to prescribe, order, give, or administer any drug or medicine for the use of any other individual. Offering or undertaking to prevent or diagnose, correct, prescribe for, administer to, or treat in any manner or by any means, methods, or devices any disease, illness, pain, wound, fracture, infirmity, defect, or abnormal physical or mental condition of any individual, including the management of pregnancy or parturition.
This means that diagnosing and treating diseases is a significant part of practising medicine in North Carolina. Only individuals with an active license or approval from the NCMB are authorised to do so. These include physicians, physician assistants, and nurse practitioners.
The NCMB also recognises an exception to the prohibition on the corporate practice of medicine for non-profit hospitals and medical practices owned by such hospitals. This is because non-profit hospitals share the same mission as the Board in protecting the well-being of North Carolina citizens. As such, hospital-owned practices are expected to recognise the ethical obligations of their licensed employees to their patients and allow them to discharge such obligations.
The Board regularly investigates and sanctions licensees for violations of North Carolina's actively enforced corporate practice of medicine prohibition. This includes scenarios where a non-licensed entity employs physician assistants or nurse practitioners who are supervised by a third-party physician. Such arrangements may be deemed unlawful "straw" practices, where the licensee is essentially "renting" their license to a non-licensed business.
Sedition Act of 1789: Unconstitutional Violation?
You may want to see also
Explore related products

Performing surgery
The North Carolina Medical Board (NCMB) has outlined specific guidelines for performing surgery in the state, which fall under the Medical Practice Act (MPA) or Chapter 90 of the NC General Statute on medicine and allied health occupations. Here are the key details regarding the performance of surgery in North Carolina:
Qualifications and Licensing:
To legally perform surgery in North Carolina, an individual must hold an active, non-limited license to practice medicine in the state. This license is granted by the North Carolina Medical Board. Additionally, the individual must have an active clinical or teaching practice, defined as involving patient care, instruction of students, or clinical research for at least 20 hours per week. They must also have actively practiced in North Carolina for at least five consecutive years preceding their appointment and intend to remain in active practice in the state.
Office-Based Surgical Procedures:
The NCMB has established guidelines for office-based surgical procedures to ensure patient safety and provide criteria for evaluating the conduct of licensees. These guidelines include:
- Direct observation of the patient and their responses to verbal commands.
- Continuous pulse oximetry or an alternative method of measuring oxygen saturation if clinically effective.
- Continuous use of an electrocardiogram monitor.
- Frequent monitoring of the patient's vital signs, including blood pressure, pulse rate, and respirations, recorded at least every five minutes.
- Continuous body temperature measurement for pediatric patients.
- Intraoperative monitoring findings must be documented in the patient's medical record.
- Postoperative care: The surgeon or licensee performing the procedure should evaluate the patient immediately upon completion of the surgery and anesthesia.
- Personnel requirements: The licensee performing the surgery should be ACLS certified, and at least one other healthcare professional should be BLS certified. If anesthesia services are provided to infants and children, personnel should be appropriately certified to handle pediatric emergencies (APLS or PALS certified).
- Malpractice insurance coverage for surgical procedures performed in the office.
- Procedure-specific competence: This includes education, training, experience, and evaluation. Training should include a didactic course complemented by hands-on, observed experience, followed by a specified number of supervised cases by a licensed healthcare professional competent in the respective procedure.
Medical School Faculty License:
A physician who holds a full-time faculty appointment at a North Carolina medical school can obtain a medical school faculty license to practice medicine and surgery. However, their practice is limited to the confines of the medical school and its affiliates. Practicing beyond these limitations is considered a Class 3 misdemeanor, subject to fines.
Disciplinary Action:
The NCMB regularly investigates and takes action against unlawful practice, including aiding the unlicensed practice of medicine through improper practice ownership arrangements. Disciplinary action can also be taken against licensees who fail to comply with the established guidelines for office-based procedures or engage in unethical practices such as "straw ownership" of medical practices.
Understanding Citizenship: The Constitution's Definition Explained
You may want to see also

Corporate practice of medicine
The Corporate Practice of Medicine (CPOM) laws in North Carolina prohibit standard corporations or other non-physician entities from practising medicine or employing practising physicians. The North Carolina Medical Board enforces these laws, which aim to ensure that medical decisions are based solely on patient care and are not influenced by corporate interests.
The North Carolina Professional Corporations Act (N.C. Gen. Stat. ¶55B, et. seq.) requires corporations providing professional services to be owned entirely by licensees of that profession. Medical practices must therefore be owned by licensed physicians, or in some cases, a combination of other authorised clinicians. The Board may take disciplinary action against licensees providing medical services on behalf of businesses engaged in the corporate practice of medicine.
The Board does recognise certain exceptions to the CPOM, including hospitals, health maintenance organisations, and non-profit hospitals and medical practices owned by such hospitals. These exceptions are based on the policy that non-profit hospitals are charged with the same mission as the Board in protecting the well-being of North Carolina citizens.
The CPOM laws also address issues such as "straw ownership" of medical practices, where a licensed physician is made the sole shareholder of a practice controlled and operated by a non-physician. In such cases, the physician straw owner can face disciplinary action for aiding and abetting the unlicensed practice of medicine.
Overall, the CPOM laws in North Carolina aim to protect the physician-patient relationship from commercial influence and ensure that medical decisions are made in the best interests of patient care.
Legislative Branch: Powers and Main Functions Explained
You may want to see also
Frequently asked questions
The Medical Practice Act (MPA) is chapter 90 of the NC General Statute on medicine and allied health occupations.
The practice of medicine or surgery in North Carolina includes:
- Advertising or representing oneself as authorized to practice medicine in the state.
- Prescribing, ordering, giving, or administering drugs or medicine to another individual.
- Preventing, diagnosing, correcting, prescribing for, treating, or administering to any disease, illness, pain, wound, or any other physical or mental condition in another individual.
- Performing any surgical procedure on an individual.
Yes, the Board recognizes an exception for non-profit hospitals and medical practices owned by such hospitals. This exception is based on the shared mission of protecting the well-being of North Carolina citizens.
The NCMB is responsible for investigating and sanctioning licensees who violate North Carolina's corporate practice of medicine prohibition. They have published guidance on unlawful "straw" practices and the potential implications of physician supervision of individuals employed by non-licensed entities.








![The University of North Carolina Record. The School of Medicine. [1936]; no.300](https://m.media-amazon.com/images/I/61j9qgKhfbL._AC_UY218_.jpg)