Medicare Advantage Plans, also referred to as Medicare Part C, are health plans offered by private companies that contract with Medicare. These plans provide an alternative to Original Medicare, allowing enrollees to access health coverage through provider networks. Medicare Advantage Plans typically include Part A (Hospital Insurance) and Part B (Medical Insurance) benefits, with most plans also offering drug coverage (Part D). The plans can be local or regional, serving one or multiple counties or a group of states. Enrollees in these plans may be required to obtain prior approval for certain treatments or services and are generally limited to in-network providers.
| Characteristics | Values |
|---|---|
| Types of Medicare Advantage Plans | Health Maintenance Organizations (HMOs), Preferred Provider Organizations (PPOs), Special Needs Plans (SNPs), Medicare Medical Savings Accounts (MSAs), Private Fee-for-Service Plans (PFFS) |
| Provider Networks | Limited to doctors, hospitals, and providers within the plan's network |
| Enrollment | Over 6 million beneficiaries enrolled in Special Needs Plans in 2023; 5.5 million in Employer Group Plans |
| Prior Authorization | Required for some treatments or services; plans can approve or deny care based on medical research and standards |
| Drug Coverage | Most plans include Part D coverage; cannot usually join a separate Medicare drug plan |
| Service Area | Coverage may be limited to specific counties or states |
Explore related products
What You'll Learn

Medicare Advantage Plans are offered by private companies
Medicare Advantage Plans, also known as Medicare Part C, are offered by private companies that contract with Medicare. These companies must follow the rules set by Medicare, and the plans are subject to Medicare's oversight.
Medicare Advantage Plans have been available since the 1970s, but their popularity has increased significantly due to changes made by the Medicare Modernization Act of 2003 and the Affordable Care Act (ACA). The plans provide an alternative to Original Medicare, combining Part A (Hospital Insurance) and Part B (Medical Insurance) benefits.
Most Medicare Advantage Plans include drug coverage, often referred to as Part D. This coverage is included in the plan, and enrollees typically cannot join a separate Medicare drug plan. The plans cover a range of brand-name and generic prescription drugs, with costs varying based on the specific drug and its assigned tier.
Medicare Advantage Plans offer access to providers through specific networks of doctors, hospitals, and other health providers. These networks can be more limited than traditional Medicare, and enrollees typically need to use in-network providers to receive coverage. The breadth of these networks can vary, and the Centers for Medicare and Medicaid Services (CMS) has stated that it will strengthen its oversight of plan networks to ensure compliance with "network adequacy" standards.
It's important to note that Medicare Advantage Plans have certain enrolment requirements and restrictions. For example, moving outside the plan's service area or losing Medicare eligibility can result in disenrolment. Additionally, joining a Medicare Advantage Plan may impact employer or union coverage for both the enrollee and their dependents.
Constitutional Lawyers: Bar Exam Essential?
You may want to see also

Most plans include drug coverage (Part D)
Medicare Advantage Plans, also known as Medicare Part C, are offered by Medicare-approved private companies that must follow rules set by Medicare. These plans are an alternative to Original Medicare and provide Part A (Hospital Insurance) and Part B (Medical Insurance) benefits.
Most Medicare Advantage Plans include drug coverage, known as Part D. This coverage is included in the plan, and enrollees typically cannot join a separate Medicare drug plan. The plans cover a range of brand-name and generic prescription drugs, with each plan having a specific list of covered drugs called a "formulary." The drugs on the formulary are divided into tiers based on cost, with lower-tier drugs costing less than higher-tier ones.
It is important to note that Medicare Advantage Plans have specific provider networks for doctors, hospitals, and other health providers. These networks can vary in breadth, and access to reliable information on them may be challenging for enrollees and their families. While Medicare Advantage Plans offer access to providers within their networks, traditional Medicare allows beneficiaries to access any doctor or hospital that accepts Medicare across the United States.
Additionally, Medicare Advantage Plans typically require prior approval or authorization for coverage of certain treatments or services. This means that plans can approve or deny care based on medical research and standards before or even after the service is received, provided they follow Medicare rules and guidelines.
Medicare Advantage Plans provide an alternative option for health coverage, and with most plans including drug coverage, beneficiaries can have their medical and prescription drug needs addressed through their chosen plan.
Contract Breaches: Understanding Non-Performance
You may want to see also

Prior approval is required for some treatments
Medicare Advantage plans are private plans that have been an option in Medicare since the 1970s. In 2023, there were 6 million beneficiaries enrolled in Special Needs Plans, which are Medicare Advantage plans designed for people with high healthcare needs.
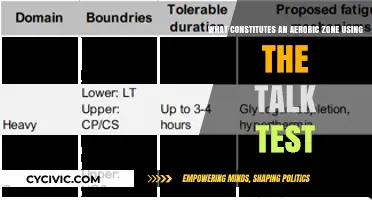
Nearly all Medicare Advantage enrollees are required to obtain prior approval, or authorization, for coverage of some treatments or services. This is in contrast to traditional Medicare, which rarely requires prior authorization. Prior authorization is required to see specialists, get out-of-network care, get non-emergency hospital care, and more. Each Medicare Advantage plan has different requirements, so enrollees should contact their plan to ask when/if prior authorization is needed.
Prior authorization requirements are intended to ensure that health care services are medically necessary by requiring approval before a service or other benefit is provided. However, prior authorization processes can result in administrative hassles for providers, delays for patients in receiving necessary care, and in some instances, denials of medically necessary services.
In 2023, Medicare Advantage insurers made nearly 50 million prior authorization determinations, reflecting steady year-over-year increases since 2021. In the same year, insurers fully or partially denied 3.2 million prior authorization requests, which is a somewhat smaller share (6.4%) of all requests than in 2022 (7.4%).
While prior authorization can help plans control costs and allow patients and providers to make informed decisions, it can also be overused or misused, resulting in inappropriate barriers to needed care. Widespread reports detailing such enrollee and provider experiences in Medicare Advantage indicate prior authorization abuses are happening at an enormous scale.
Charity or Terrorism: The Legal Line on Donations
You may want to see also
Explore related products

Medicare Advantage Plan enrollees can access providers through limited networks
Medicare Advantage Plans, also known as Medicare Part C, are offered by private companies that contract with Medicare. These plans provide an alternative to Original Medicare for individuals seeking health and drug coverage. While Original Medicare allows beneficiaries to see any doctor or utilise any hospital that accepts Medicare across the United States, Medicare Advantage Plans operate through limited provider networks. This means that enrollees can only access healthcare providers, such as doctors, hospitals, and other health providers, within their specific network.
Medicare Advantage Plans typically fall into two categories: Health Maintenance Organizations (HMOs) and Preferred Provider Organizations (PPOs). HMOs generally provide coverage solely for in-network care, restricting beneficiaries to a predetermined network of healthcare providers. Conversely, PPOs offer more flexibility, allowing enrollees to utilise out-of-network providers at a higher cost. PPOs can be local, serving one or multiple counties, or regional, covering a single state or group of states.
The limited provider networks of Medicare Advantage Plans can vary significantly in terms of the number of included physicians. For instance, a 2017 analysis revealed that Medicare Advantage networks, on average, encompassed fewer than half (46%) of all Medicare physicians within a given county. This variation in network size underscores the importance of enrollees understanding the specifics of their chosen plan's network. However, obtaining reliable information about plan networks can be challenging for enrollees and their family members.
The Centers for Medicare and Medicaid Services (CMS), which administers Medicare Advantage Plans, has recognised the need for improved oversight of plan networks. Beginning in 2024, CMS intends to strengthen its supervision, addressing instances of non-compliance with "network adequacy" standards. While narrow-network plans may offer advantages in controlling costs and managing quality, broader networks are also promoted by some Medicare Advantage Plans. Ultimately, the impact of network size on the quality of care remains unclear, and individuals must carefully consider their healthcare needs when selecting a Medicare Advantage Plan.
Understanding Subpart Definition in Federal Rule of Procedure 33(a)
You may want to see also

Special Needs Plans are designed for people with high healthcare needs
Medicare Advantage Plans are an alternative to Original Medicare, and most are either HMOs or PPOs. Medicare Advantage Plans include Special Needs Plans (SNPs), which are designed for people with high healthcare needs. SNPs are a type of Medicare Advantage Plan that serves individuals with chronic or disabling conditions. These plans require eligible patients to receive care and services from doctors or hospitals in their Medicare SNP networks.
There are three kinds of Special Needs Plans: Dual Special Needs Plans (D-SNPs), Chronic Special Needs Plans (C-SNPs), and Institutional Special Needs Plans (I-SNPs). D-SNPs are for people who have both Medicare and Medicaid, C-SNPs are for people living with severe or disabling chronic conditions, and I-SNPs are for people who live in a skilled nursing facility. Additionally, a person who lives in a contracted assisted living facility and needs the same kind of care as those who live in a skilled nursing facility may qualify for an Institutional-Equivalent Special Needs Plan (IE-SNP).
To qualify for a D-SNP, you must receive Original Medicare (Parts A and B) and full Medicaid benefits. Depending on the amount of Medicaid benefit received, one might be considered "full dual-eligible" or "partial dual-eligible". Most individuals who qualify will receive a letter from their state Medicaid office. Some of the extra benefits Dual Special Needs Plans typically include are dental, vision and hearing coverage, care coordination via a personal care coordinator, personal emergency response systems (PERS), and telehealth options such as virtual medical visits with your doctor.
C-SNPs are designed for people with specific severe and chronic diseases or certain healthcare needs. There are 15 SNP-specific chronic conditions approved by the Centers for Medicare and Medicaid Services (CMS), including autoimmune disorders, cancer, cardiovascular disorders, severe hematologic disorders, and more. SNPs include care coordination services and tailor their benefits, provider choices, and list of covered drugs (formularies) to best meet the specific needs of the groups they serve. For example, if you have a severe condition and need a hospital stay, an SNP may cover extra days in the hospital.
California Bar Exam: Constitutional Criminal Procedure Frequency
You may want to see also
Frequently asked questions
Medicare Advantage Plans (also referred to as Medicare Part C) are health plans offered by private companies that contract with Medicare. These plans provide Part A (Hospital Insurance) and Part B (Medical Insurance) benefits to people with Medicare.
There are several types of Medicare Advantage Plans, including Health Maintenance Organizations (HMOs), Preferred Provider Organizations (PPOs), Special Needs Plans (SNPs), Medicare Medical Savings Accounts (MSAs), and Private Fee-for-Service Plans (PFFS). HMOs generally cover only in-network care, while PPOs offer access to out-of-network providers at a higher cost.
To enroll in a Medicare Advantage Plan, you must first have Medicare Part A and Part B. You can then choose a plan offered by a Medicare-approved private company. Remember to talk to your employer, union, or benefits administrator about their rules before joining, as it may affect your existing coverage.