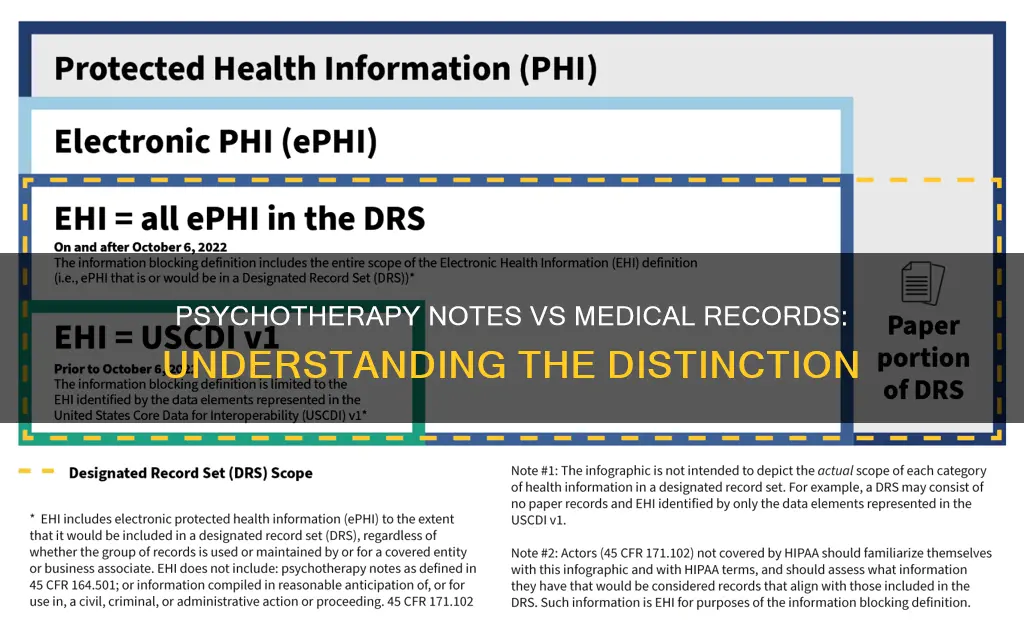
Psychotherapy notes are private notes recorded by a mental health professional documenting or analyzing the contents of a session. They are not shared with other healthcare professionals or insurers and are kept separately from the client's medical record. Psychotherapy records, on the other hand, are mental health records that therapists must maintain for every client. These records are part of the client's formal medical record and can be shared with other healthcare providers involved in the client's care. While psychotherapy notes are optional and private, psychotherapy records are essential and required by law.
| Characteristics | Values |
|---|---|
| Privacy | Psychotherapy notes are private and confidential, meant for the therapist alone and are not disclosed to anyone except the therapist. Progress notes are part of a client's medical record and are private but can be shared with other healthcare providers involved in the client's care. |
| Legality | Psychotherapy notes are not required by law. Progress notes are required by law. |
| Storage | Psychotherapy notes should be stored separately from the patient's general medical record. |
| Content | Psychotherapy notes can be in any medium, including personal shorthand, and can contain a clinician's thoughts, impressions, and feelings about a session, along with important details and reminders. Progress notes capture the course of treatment in a standardized way, including session start and stop times, summaries of symptoms, diagnosis, prognosis, and treatment plans. |
| Access | Psychotherapy notes require specific authorization for release, such as a court order, subpoena, or request from a government agency. Progress notes require a release of information from the patient to be accessed by other medical team providers. |
Explore related products
$12.99 $12.99
$47.14 $67.95
What You'll Learn
- Psychotherapy notes are optional, private notes, while progress notes are required by law
- Psychotherapy notes are not shared with other healthcare professionals, insurers, or clients
- Progress notes are part of a client's formal medical record
- Psychotherapy notes are subject to greater privacy and confidentiality
- Psychotherapy notes can be disclosed in response to a court order, subpoena, or law enforcement inquiry

Psychotherapy notes are optional, private notes, while progress notes are required by law
Psychotherapy notes are detailed, private notes recorded by mental health professionals. They are not required by law and are kept separate from the client's medical record. These notes are meant for the therapist alone and are subject to greater privacy and confidentiality. They can be in any medium, including personal shorthand, scribbled notes, or electronic records. Psychotherapy notes are optional and often contain the therapist's thoughts, impressions, feelings, and important details from the session. They can also include ideas, hunches, and questions for supervision. Therapists must obtain consent from their clients for any use or disclosure of these notes.
In contrast, progress notes are required by law and constitute a part of the client's formal medical record. They capture the standardised course of treatment, including the client's diagnosis, response to treatment, and any interventions. Progress notes are shared with other healthcare professionals involved in the client's care and are HIPAA-protected. They are stored securely within the patient's medical chart.
Psychotherapy notes are granted exceptional protection under HIPAA and are generally not disclosed to anyone except the therapist. They are considered separate pieces of information from the client's medical record and are subject to different privacy protections. While clients may request access to their psychotherapy notes, therapists have the right to refuse access to maintain the privacy and confidentiality of the therapeutic relationship.
It is important to note that psychotherapy notes may be disclosed in certain legal situations, such as a court order, subpoena, or law enforcement inquiry. However, companies or employers cannot request these notes during an audit of patient records. Therapists should obtain written permission from clients before keeping or destroying notes no longer required for treatment. Proper handling of these notes is crucial for maintaining trust and complying with legal and ethical guidelines.
Constitution Party: Core Beliefs Explored
You may want to see also

Psychotherapy notes are not shared with other healthcare professionals, insurers, or clients
Psychotherapy notes are private notes recorded by a mental health professional. They document or analyse the contents of a session and can take any form, including personal shorthand, scribbled notes, or any format that makes sense to the therapist. They are not shared with other healthcare professionals, insurers, or clients. They are separate from the client's medical record and are not required by law. They are for the therapist's eyes only and are subject to greater privacy and confidentiality.
These notes are often referred to as process or private notes and are kept separate from the client's psychotherapy records. They are not meant to be shared and are optional, unlike progress notes, which are a legal requirement. Psychotherapy notes are the therapist's private thoughts, impressions, and feelings about a session, along with important details and reminders to continue particular themes or topics. They can include ideas, hunches, and questions to explore in supervision.
The privacy and confidentiality of these notes are protected by HIPAA, and they are usually disclosed only to the therapist. In contrast, progress notes are part of a client's formal medical record and can be shared with other healthcare providers involved in the client's care. Psychotherapy notes are not meant to be shared with other healthcare professionals as they contain sensitive information that could be misused if accessed by unauthorized individuals.
While clients may request access to their psychotherapy notes, therapists may refuse access to these notes, which are kept separate from the client's medical records. Therapists must obtain written consent from their clients before disclosing psychotherapy notes, and even then, they have the right to deny access if it could harm the client. Psychotherapy notes are granted exceptional protection under HIPAA, and while there are rare cases where a court can request these notes, they are generally kept strictly confidential.
Understanding Full-Time Hours for Occupational Therapists
You may want to see also

Progress notes are part of a client's formal medical record
Psychotherapy notes are private notes recorded by a mental health professional. They document or analyse the contents of a therapy session and can include the therapist's thoughts, impressions, and feelings about the session. They are not required by law and are kept separate from the client's medical record. Psychotherapy notes are optional and are not meant to be shared with other healthcare professionals or insurers. They are subject to a greater degree of privacy and confidentiality and are protected by HIPAA laws, which state that even clients do not have the right to access them without providing written consent.
Progress notes, on the other hand, are a part of a client's formal medical record. They capture the course of treatment in a standardised way, allowing other medical professionals to understand the client's diagnosis, response to treatment, and any interventions made. Progress notes are required by law and are also HIPAA-protected, requiring secure storage and limited access. Any access to the client's medical record by someone other than the therapist requires a release of information on file from the patient.
While psychotherapy notes are private and meant solely for the therapist's reference, progress notes are intended to be shared with other healthcare providers involved in the client's care. They form the client's medical record and are essential for providing a comprehensive understanding of the client's treatment progress and overall health status.
The distinction between psychotherapy notes and progress notes highlights the importance of maintaining detailed and accurate records in mental health practices. Psychotherapy notes allow therapists to explore treatment options and process challenging cases, while progress notes ensure continuity of care and facilitate collaboration among healthcare professionals.
It is crucial for therapists to obtain proper consent and adhere to legal and ethical guidelines when handling sensitive client information, whether in the form of psychotherapy notes or progress notes.
Congress' Constitutional Powers: Lawmaking and Oversight
You may want to see also
Explore related products
$28.02 $59.99

Psychotherapy notes are subject to greater privacy and confidentiality
The Health Insurance Portability and Accountability Act (HIPAA) Privacy Law distinguishes between mental health records, which are part of a patient's overall medical record, and psychotherapy notes, which are granted exceptional protection and treated as separate pieces of information. Psychotherapy notes are generally not disclosed to anyone except the therapist, and even clients do not have the right to access them. They are meant to provide a safe space for therapists to document their thoughts and impressions without concern for external judgment or scrutiny, allowing for more comprehensive and effective therapy.
While psychotherapy notes are generally protected from disclosure, there are rare exceptions. In the case of a court order, subpoena, summons, request from a government agency, or law enforcement inquiry, therapists may be legally required to release their notes. Additionally, during treatment by another provider, notes may be requested to facilitate continuity of care, and therapists have the right to deny access if it could harm the client.
It is important to obtain written permission from the client before keeping or destroying notes no longer required for treatment. Properly shredding paper notes and permanently deleting electronic files are essential to prevent unauthorised access. Maintaining the privacy and confidentiality of clients' personal information is crucial for therapists to build trust and comply with legal and ethical guidelines.
Gastro or Constitutional: Loss of Appetite in ROS
You may want to see also

Psychotherapy notes can be disclosed in response to a court order, subpoena, or law enforcement inquiry
Psychotherapy notes are private notes recorded by a mental health professional that document or analyse the contents of a session. They are not required by law and are not part of a client's official medical record. They are meant for the therapist alone and are subject to a greater degree of privacy and confidentiality. While psychotherapy notes are generally protected from disclosure, there may be certain situations in which they can be disclosed in response to a court order, subpoena, or law enforcement inquiry.
According to the U.S. Department of Health and Human Services, providers covered by HIPAA can disclose information in response to a court order. However, they can only disclose the specific information requested in the court order, and there are legal and ethical guidelines that must be followed. In the case of a subpoena, which is a formal request for information from a court or lawyer, therapists should consult with an attorney before releasing any information. While subpoenas can be tricky to deal with due to the extra privacy rules surrounding psychotherapy notes, it is important to remember that psychotherapy notes can be subpoenaed, although it is rare.
If a therapist receives a court order or subpoena, they must first determine what information is being requested and then review the applicable laws and ethical guidelines to understand what can be released. Therapists should also consider obtaining separate authorization from the client to release psychotherapy notes, as required by HIPAA law. Additionally, therapists have a responsibility to not release any information that could be harmful to the client, even with the patient's permission. In such cases, a court order may be required, and the judge must believe that the records are necessary for the case.
While psychotherapy notes can be disclosed in specific circumstances, it is important to prioritise protecting client privacy. Therapists should store psychotherapy notes securely and separately from the client's medical record to ensure confidentiality. Furthermore, therapists should obtain written permission from the client before keeping or destroying notes that are no longer required for treatment. Proper handling of client requests for access to their psychotherapy notes is also crucial for maintaining trust and complying with legal and ethical guidelines. Overall, while disclosure of psychotherapy notes may be required in certain legal situations, therapists should be mindful of their client's privacy and well-being throughout the process.
Centinel's Objections: A Federal Constitution Critique
You may want to see also
Frequently asked questions
Psychotherapy notes are private notes recorded by a mental health professional documenting or analyzing the contents of a session. They are also known as private or process notes and often contain a clinician's thoughts, impressions, and feelings about a session.
Psychotherapy notes are separate from the client's medical records and are not shared with other healthcare providers. They are optional, private notes made by the therapist, whereas medical records are required by law and include information such as intake forms, assessments, diagnoses, and treatment plans.
Clients generally do not have the right to access their therapist's private psychotherapy notes. However, state laws may vary, and it is important to check the specific laws in your state.
Yes, psychotherapy notes may be disclosed in response to a court order, subpoena, summons, request from a government agency, or law enforcement inquiry. Therapists must obtain written consent from their clients before disclosing any information.
Psychotherapy notes allow therapists to explore treatment options and process challenging cases effectively. They provide a more comprehensive understanding of the client's unique situation and enhance the therapist's ability to provide targeted treatment.