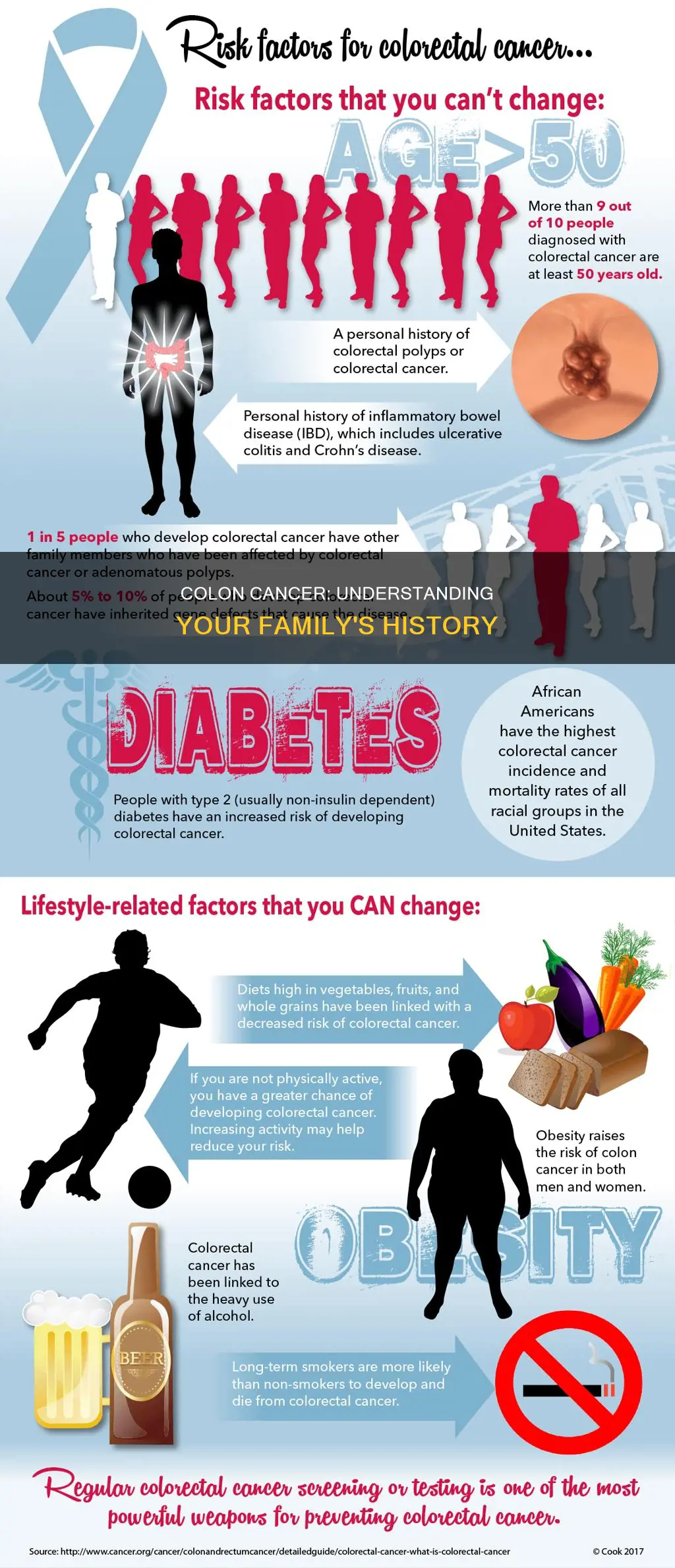
A family history of colon cancer can be a valuable tool in understanding your risk of developing the disease. Colon cancer can run in families due to genetic factors, and having a first-degree relative (parent, sibling, or child) diagnosed with colon cancer increases an individual's risk. If a first-degree relative was diagnosed at a young age, the risk is even higher. Other factors, such as a family history of adenomatous polyps and inherited syndromes like Lynch syndrome, can also contribute to an increased risk. Understanding your family history allows you to take preventive measures, undergo genetic counseling, and consider earlier and more frequent screenings, such as colonoscopies, to detect and prevent colon cancer.
| Characteristics | Values |
|---|---|
| Family history of colorectal cancer | A family history of colorectal cancer puts an individual at a higher risk of developing the disease. |
| First-degree relative with colorectal cancer | If a first-degree relative (parent, sibling, or child) has a history of colorectal cancer, the risk is even higher. |
| Age of diagnosis in first-degree relative | If the first-degree relative was diagnosed before the age of 50, the risk is significantly increased. |
| Multiple first-degree relatives with colorectal cancer | If more than one first-degree relative is affected, the risk is further elevated. |
| Age of onset of screening | Individuals with a family history of colorectal cancer are advised to start screening at an earlier age, typically around 40 or 10 years earlier than the age of diagnosis of their relative, whichever is earlier. |
| Screening frequency | More frequent screenings may be recommended for those with a family history. |
| Family history of pre-cancerous polyps | A family history of pre-cancerous colorectal polyps (adenomatous polyps) is also considered a risk factor. |
| Inherited syndromes | Lynch syndrome and familial adenomatous polyposis (FAP) are the most common inherited syndromes linked to colorectal cancers. |
| Genetic testing | Genetic counseling and genetic testing are suggested for individuals with a strong family history of colorectal cancer, especially if cancers occur at a young age. |
Explore related products
What You'll Learn

First-degree relatives with colon cancer
Having a first-degree relative with colon cancer is a significant indicator of inherited risk. First-degree relatives include parents, siblings, and children. If you have a first-degree relative who was diagnosed with colon cancer, it is recommended that you consult a doctor about the possibility of starting screening at an earlier age. The recommended age for starting colorectal cancer screenings is typically 45, but those with a family history of the disease may benefit from beginning at 40 or 10 years earlier than the age of diagnosis of the relative, whichever is earlier. For example, if your parent was diagnosed with colon cancer at 35, you should consider starting screenings at 25.
The risk associated with having a first-degree relative with colon cancer is even higher if the relative was diagnosed before the age of 50. In such cases, the risk for first-degree relatives of being diagnosed with colorectal cancer before the age of 50 is six times higher than average. Additionally, if more than one first-degree relative has been affected, the risk is further increased.
It is important to be aware of your family's medical history, including extended family, and to share this information with your physician. This can help determine if you are at an increased risk and whether preventive measures or more frequent screenings are necessary.
If you have a first-degree relative with colon cancer, it is recommended that you gather information about your family's medical history and consult a genetic counselor to assess your potential risks. This can be a powerful tool in preventing and detecting cancer early.
How New Jersey's Support Shaped the US Constitution
You may want to see also

Family history of adenomatous polyps
A family history of adenomatous polyps is a risk factor for developing colorectal cancer. Adenomatous polyps are pre-cancerous growths in the colon or rectum that can turn cancerous. If you have a first-degree relative (parent, sibling, or child) with a history of these polyps, you are at a higher risk of developing colorectal cancer. This risk is further elevated if your relative was diagnosed with polyps before the age of 50, or if multiple first-degree relatives are affected.
The presence of adenomatous polyps in the family can be due to inherited genetic factors, such as Lynch syndrome or familial adenomatous polyposis (FAP). Lynch syndrome accounts for about 2% to 4% of colorectal cancers and is caused by an inherited defect in specific genes, including MLH1, MSH2, MSH6, PMS2, and EPCAM. People with Lynch syndrome tend to develop colorectal cancer at a younger age and usually on the right side of the colon. While those affected by Lynch syndrome can have polyps, they tend to have only a few.
On the other hand, FAP is caused by changes or mutations in the APC gene inherited from parents. FAP is responsible for about 1% of colorectal cancers. In the most common form of FAP, hundreds or even thousands of polyps develop in the colon and rectum, often starting at a young age, between 10 and 12 years old. By the time they reach 40, almost all individuals with FAP will have developed colon cancer if their colon has not been removed preventively. FAP also increases the risk of cancers in other organs, including the stomach, small intestines, pancreas, and liver.
If you have a family history of adenomatous polyps, it is important to consult your doctor about the need for earlier and more frequent colorectal cancer screening. Colonoscopies are recommended for patients with a family history of pre-cancerous polyps, as they allow for direct visualisation and examination of the entire colon. During this procedure, any polyps that are found can be removed. Additionally, individuals can utilise online tools such as My Family Health Portrait to comprehensively document their family health history and improve the management of preventive care.
Republicans' Union: Restoring the Constitution During Reconstruction
You may want to see also

Lynch syndrome
If you have a Lynch syndrome diagnosis, your healthcare provider will offer regular tests to check for cancer, including a colonoscopy, transvaginal ultrasound, urinalysis, and tumour biopsy. Colonoscopies are recommended to begin at age 20 to 25 and repeat every 1 to 2 years, or 5 years younger than the youngest person diagnosed with cancer in your family.
If you have a first-degree relative (parent, sibling, or child) diagnosed with colon cancer, especially at a young age, it is recommended that you start getting screened at age 40 or 10 years earlier than your relative's diagnosis, whichever is earlier. If your family member was diagnosed before the age of 50, it is a significant indicator of inherited risk and you should consider collecting your family history and consulting a genetic counsellor.
Silver Dollar Value: 1982 Constitution Coin Worth
You may want to see also
Explore related products

Familial adenomatous polyposis (FAP)
The most common form of FAP usually presents with a large number of polyps, ranging from hundreds to thousands, and can develop in both children and adults. If left untreated, these polyps can become cancerous. The age of onset varies, but it often starts in early adolescence, with cancer typically developing by early adulthood. In some cases, FAP can develop "'silently'", with few or no signs or symptoms until it has progressed to advanced colorectal cancer. This makes early detection and screening crucial for individuals at risk.
The second form of FAP, known as attenuated FAP or AFAP, is a milder variant with a slightly impaired but still functional APC gene. Individuals with this form of FAP typically develop fewer polyps, usually fewer than 100, and the onset of colorectal cancer tends to occur later in life, typically in the 40s to 70s. However, even with fewer polyps, the lifetime risk of cancer remains high at around 70%.
The third variant is autosomal recessive familial adenomatous polyposis or MUTYH-associated polyposis, which is also a milder form. This variant requires both parents to be carriers for the condition to manifest. Genetic testing, such as a blood test for the APC gene mutation, is available to help diagnose FAP and assess the risk of developing colorectal cancer.
FAP is one of the most common inherited syndromes linked to colorectal cancers, accounting for about 1% of all colorectal cancer cases. It is important for individuals with a family history of FAP or colorectal cancer to undergo regular screening and consult with a healthcare professional to determine their risk and preventive measures.
Federal Programs: Unconstitutional and Unaccounted For
You may want to see also

Age of diagnosis
When assessing family history as a risk factor for colorectal cancer, the age of diagnosis of affected relatives is an important consideration. Early-onset colorectal cancer, which is typically defined as a diagnosis before the age of 50, is often associated with a stronger genetic predisposition.
If a first-degree relative (parent, sibling, or child) has been diagnosed with colorectal cancer at a young age, it may indicate an increased risk for other family members. The risk is generally higher if the affected relative was diagnosed at a younger age, especially if the cancer occurred
Disney: The American Experience's Magic Maker
You may want to see also
Frequently asked questions
A family history of colon cancer means that you have an immediate family member or multiple other close family members who have had colon cancer. This includes parents, siblings, and children.
A family history of colon cancer puts you at a higher risk of developing the disease. The risk is even higher if a first-degree relative was diagnosed at a younger age, typically considered to be under 50 or 60 years old.
If you have a family history of colon cancer, it is important to talk to your doctor and undergo appropriate screening tests, such as a colonoscopy. You may also benefit from earlier and more frequent screenings, as well as genetic counseling to assess your personal risk.
The most common inherited syndrome linked with colon cancer is Lynch syndrome, which accounts for about 2-4% of all colorectal cancers. Familial adenomatous polyposis (FAP) is another syndrome caused by mutations in the APC gene, contributing to about 1% of colorectal cancers.