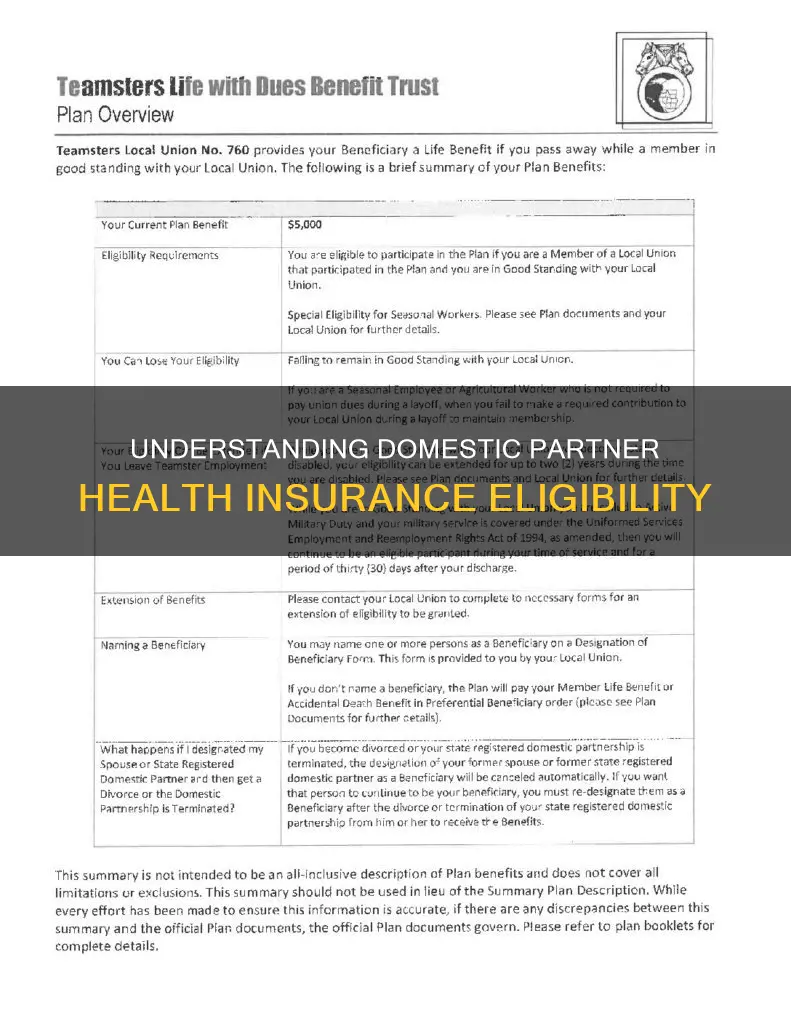
Domestic partner health insurance is when health insurance benefits are extended to a domestic partner, much like they often are to married spouses. However, there is no federal definition or recognition of domestic partnerships, nor guidelines for the legal rights and benefits that come with it. This means that whether you’re eligible to be categorized as being in a domestic partnership depends on where you live and your health plan's rules. Insurance companies typically require partners to have cohabited for 6-12 months, be unmarried and not in another domestic partnership, be unrelated by blood, and be financially interdependent. Employers can choose to offer domestic partnership health insurance benefits and set their own eligibility rules, but they are not required to do so. If they do, they must follow federal, state, and local laws pertaining to whether domestic partners are eligible for health insurance benefits.
| Characteristics | Values |
|---|---|
| Definition of "domestic partner" | Two unmarried and unrelated people cohabitating and sharing a domestic life |
| Legal recognition | Not recognized federally; recognized in some states and municipalities but with varying definitions and requirements |
| Proof of domestic partnership | Registration in a local domestic partnership registry, affidavit, or other documentation |
| Cohabitation requirements | 6-12 months, depending on the company's requirements |
| Financial requirements | Financial interdependence |
| Age requirements | Both partners must be at least 18 years old |
| Marital status requirements | Neither partner can be married or in another domestic partnership |
| Blood relation requirements | Unrelated by blood |
| Equality considerations | Employers should treat spouses and domestic partners equally and require the same documentation for both |
| Confidentiality | Employers should have a confidentiality policy to protect employees' privacy |
| Anti-discrimination policy | Companies offering domestic partner benefits should also have an anti-discrimination policy that includes sexual orientation |
Explore related products
What You'll Learn

The definition of a domestic partner
Generally, a domestic partnership refers to a committed relationship between two unmarried and unrelated individuals who cohabit and share a domestic life. This definition includes both same-sex and opposite-sex couples. To be recognised as domestic partners, couples typically need to meet specific criteria set by insurance companies or local governments. These criteria often include cohabitation for a certain period (ranging from 6 to 12 months), financial interdependence, and not being married or partnered with anyone else.
In the context of health insurance, domestic partner benefits may be offered by employers or insurance companies. Employers can choose to provide domestic partner health benefits even if it is not legally recognised in their state or municipality, setting their own eligibility rules. Insurance companies, on the other hand, may allow domestic partners to be included in an individual's health insurance policy, treating them similarly to married spouses.
To prove eligibility for domestic partner health insurance, various forms of documentation may be required. These can include registration in a local domestic partnership registry, an affidavit or certification of the relationship, or other legal proof of the partnership. It is important to note that the recognition of these documents can vary, and employers should strive for equality in the burden of proof required from employees.
The availability of domestic partner health insurance benefits can have significant implications, especially for same-sex couples. While same-sex marriage is now legal in all states, domestic partnerships previously provided a way for these couples to access similar benefits as opposite-sex spouses. Even today, in places where same-sex relationships may face discrimination, enrolling in these benefits could potentially out" one's partner. Thus, it is essential to consider the local laws, company policies, and privacy guarantees when navigating domestic partner health insurance options.
The Constitution Framers: Their Age and Legacy
You may want to see also

Proof of a domestic partnership
Domestic partnerships are not formally recognised by federal law in the US, so each state has its own definition. This means that the requirements for proof of a domestic partnership may vary depending on where you live. However, there are some general forms of proof that are commonly requested by employers or health insurance providers.
Firstly, it is important to note that a domestic partner is not considered a spouse under federal law. Therefore, if you elect to have your partner covered under your health insurance plan, you will likely have to pay income tax and social security payroll tax on the portion of the insurance premium that your employer contributes to.
If you are seeking to prove a same-sex relationship, government-recognised proof of your partnership should exempt you from completing a domestic partnership affidavit. This could include a partnership affidavit, a civil union, or a marriage license issued in another country.
If you are in a different-sex partnership, you may be required to provide proof of eligibility, such as a marriage license. However, employers should strive to maintain equality in the burden of proof required from eligible beneficiaries. This means that documentation should not be required of partners if it is not required of spouses.
Some common forms of proof of a domestic partnership include:
- Joint mortgage or lease agreement
- Joint ownership of residence
- Joint bank account
- Joint insurance policy
- Joint ownership or lease of a motor vehicle
- Joint utility bill
- Letters from family and friends verifying the relationship
- Proof of the same permanent residence for at least six months
- Proof of sharing the costs of running a household
It is important to note that employers may have their own specific requirements for proof of a domestic partnership, so it is recommended to check with your employer or health insurance provider directly to understand their definition of a "partner" and the specific documentation needed.
The Rule of Mary and William: Constitutional Monarchy?
You may want to see also

Privacy concerns
Secondly, enrolling in domestic partner benefits may lead to unintended disclosure of personal information, especially for LGBTQ+ individuals. If the partner's employer requires disclosure of insurance coverage sources, enrolling in a domestic partner plan could "out" the partner, potentially leading to concerns in an LGBTQ+-unfriendly workplace. Additionally, signing up for these benefits may risk disclosing the relationship to the armed services due to the documentation involved.
To address these concerns, individuals should consult with their employer about privacy guarantees and review the company's anti-discrimination and confidentiality policies. It is also advisable to seek legal counsel, particularly for foreign nationals on temporary visas, as signing a domestic partnership affidavit could impact their visa status. Furthermore, understanding the tax implications and consulting a tax professional can help individuals make informed decisions about enrolling in domestic partner benefits.
In some jurisdictions, domestic partnership affidavits may create legal obligations in the event of a relationship dissolution, such as providing financial support or dividing property. While some states have Defense of Marriage Act (DOMA) laws that prevent courts from recognizing relationships, others may allow for alimony awards based on evidence of economic dependency. Therefore, it is essential to be aware of the specific laws and potential consequences in one's jurisdiction.
Addressing Constitutional Issues: Individual Rights and Freedoms
You may want to see also
Explore related products

Tax implications
The tax implications of adding a domestic partner to one's health insurance can be complex and depend on various factors, including the type of relationship, the state of residence, and the specifics of the insurance plan. Here are some key points to consider:
Tax Treatment of Domestic Partners
The Internal Revenue Service (IRS) does not recognize domestic partnerships for federal tax purposes. This means that registered domestic partners cannot file joint federal tax returns and are not considered spouses or married for tax-related benefits. However, in community property states, certain tax rules may apply differently to domestic partners.
Taxable Income
The cost of health insurance coverage for a domestic partner is generally considered taxable income, also known as "imputed income," by the IRS. This includes both the employee's contribution and the employer's contribution to the premium. The employee must include the fair market value of the coverage in their gross income and pay income tax, payroll taxes, and withholding taxes on this amount. This is because the IRS considers health coverage for a domestic partner a taxable fringe benefit.
Tax Deductions and Exemptions
While employer contributions to a legal spouse's health premiums are typically not considered taxable imputed income, this is not the case for domestic partners. Employee or retiree premium contributions for domestic partner health benefits are paid post-tax, whereas contributions for a legal spouse are often paid pre-tax. However, in certain states like California, domestic partners may be entitled to equitable tax treatment and may be able to deduct the value of employer-paid health insurance premiums when filing a state income tax return. Additionally, if a domestic partner is a dependent as defined by the IRS, there may be tax breaks available for health-related expenses.
Self-Employed Individuals
If one of the domestic partners is self-employed and treated as an employee, they may be allowed a deduction for the cost of their health insurance paid out of community funds, according to IRS regulations.
Impact on Paycheck
Adding a domestic partner to one's health insurance will likely result in tax implications on the employee's paycheck. The portion of the premium paid by the employee for their domestic partner's coverage will be subject to income tax and payroll taxes. Additionally, the portion of the premium paid by the employer for the domestic partner's coverage will also be taxed on the employee's return.
It is important to consult with a tax professional or advisor to understand the specific tax consequences of adding a domestic partner to one's health insurance, as the rules can be intricate and vary based on individual circumstances.
Constitution Day: A US Holiday?
You may want to see also

Dependents
The definition of "dependents" in the context of health insurance and domestic partnerships can vary depending on the employer, insurance provider, and local laws. Here are some key points to note regarding dependents:
- Dependents in Domestic Partnerships: In the context of domestic partnerships, dependents can include the partner's children and other eligible dependents, similar to opposite-sex spouses. Employers should ensure that the partner's children are covered as dependents and treat them equally as they would for different-sex spouses.
- Proof of Eligibility: Employers may require proof of eligibility for dependents, such as legal documentation or government recognition of the relationship. This may include birth certificates, adoption papers, or other relevant documents.
- Same-Sex Partners and Dependents: In the case of same-sex partners, employers should strive for equality in the burden of proof required for enrollment. The California Insurance Equality Act of 2004 (AB 2208) mandates that health insurance plans in California treat spouses and domestic partners equally, including their dependents.
- Financial Interdependence: Insurance companies and employers may consider financial interdependence as a criterion for defining domestic partnerships. This could include sharing finances, joint assets, or other forms of financial dependency.
- Cohabitation Requirements: Some insurance providers and employers may require a minimum period of cohabitation, such as 6-12 months, as a condition for considering someone a dependent in a domestic partnership.
- Special Enrollment Periods: If an employer offers domestic partner health benefits, there may be special enrollment periods triggered by qualifying life events, such as the formation or dissolution of a domestic partnership. These periods allow for the addition or removal of dependents from the health insurance policy.
It's important to note that the recognition of domestic partnerships and the definition of dependents can vary across different states, counties, and cities. Therefore, it is advisable to consult the relevant local government departments and review the specific policies of the insurance provider or employer to understand their specific criteria for dependents.
Equality for All: The Constitutional Promise
You may want to see also
Frequently asked questions
A domestic partnership is where two unmarried and unrelated people cohabitate and share a domestic life. This can include same-sex and opposite-sex couples.
To be eligible for health insurance as a domestic partner, you must meet certain criteria set by insurance companies and local laws. These typically include cohabiting for 6-12 months, being unmarried or in a domestic partnership with anyone else, being unrelated by blood, and being financially interdependent.
To prove your domestic partnership, you may need a government-recognized certificate or license, a partnership affidavit, or other documentation. The specific requirements vary depending on your location and employer.