Non-obese diabetic (NOD) mice are used as an animal model for type 1 diabetes. The onset of diabetes in NOD mice is associated with hyperglycemia and insulitis, a leukocytic infiltration of the pancreatic islets. NOD mice exhibit a susceptibility to the spontaneous development of autoimmune insulin-dependent diabetes. The incidence of diabetes in these mice is influenced by both genetic and environmental factors, including housing conditions, health status, and diet. Several studies have been conducted to understand the glucose tolerance and metabolic differences in NOD mice, with a focus on the role of key genes and the kinetics of glucose levels.
| Characteristics | Values |
|---|---|
| Diabetes type | 1 and 2 |
| Onset of diabetes | Insulitis, a leukocytic infiltration of the pancreatic islets |
| Diabetes incidence | 60-80% in females and 20-30% in males |
| Diabetes onset | Occurs earlier in males, usually around one month of age |
| Insulin levels | Insulin resistance |
| Glucose levels | High glucose-induced accumulation of fructose-6-phosphate |
| Glucose tolerance | Blunted early rise in blood glucose levels |
| Insulin release | Faster and larger overall insulin release |
| Blood glucose concentration | 2 g/kg glucose, 3 g/kg glucose |
| Serum insulin concentration | 0.75 units/kg insulin, 2 units/kg insulin |
Explore related products
What You'll Learn

Insulin resistance in NOD mice
Non-obese diabetic (NOD) mice are used as an animal model for type 1 diabetes. They exhibit a susceptibility to the spontaneous development of autoimmune insulin-dependent diabetes mellitus (IDDM). The onset of diabetes in NOD mice is associated with a moderate glycosuria and a non-fasting hyperglycemia.
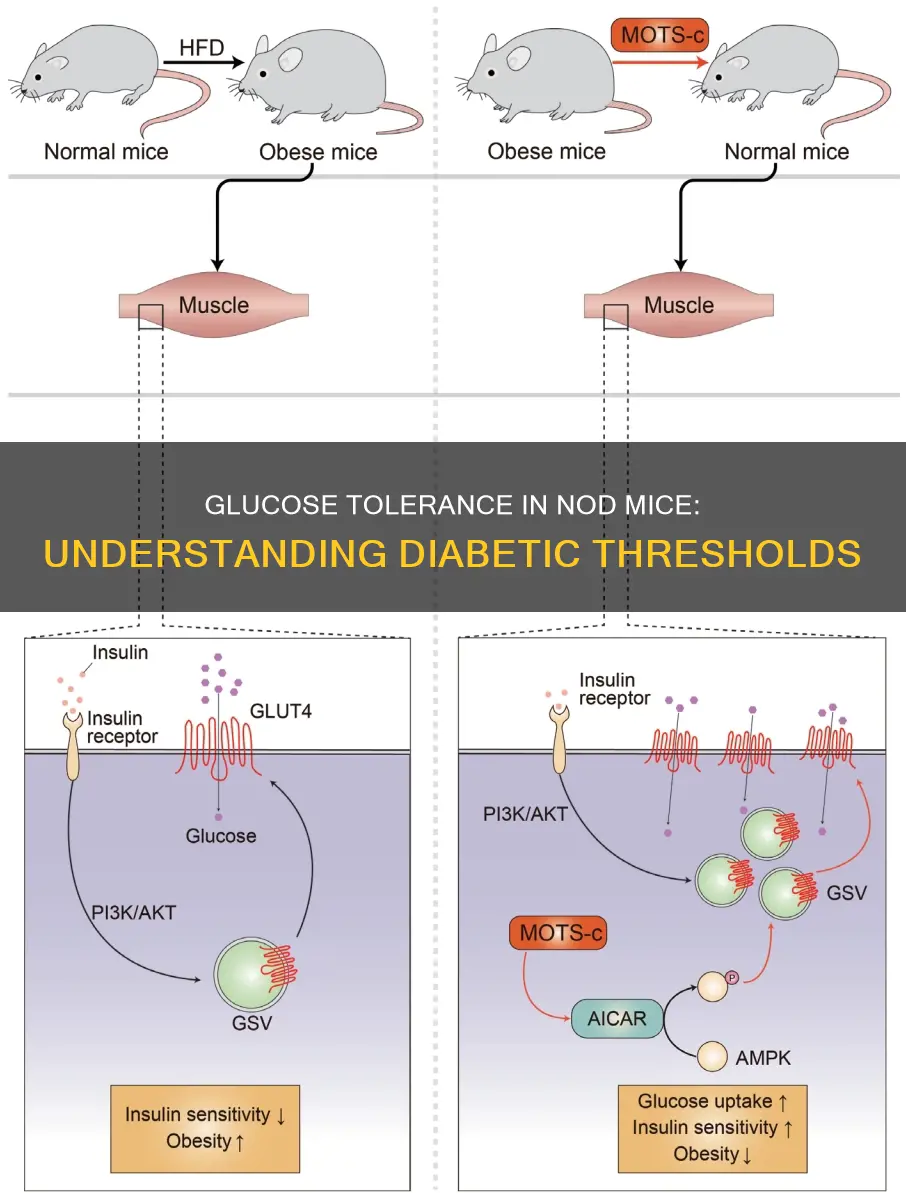
Several factors contribute to the development of diabetes in NOD mice. Firstly, they are genetically predisposed to diabetic complications, including insulin resistance, even in the absence of high circulating glucose levels and without autoimmune destruction of their β cells. This suggests that the β-cell abnormalities observed in NOD mice may be intrinsic. Additionally, NOD mice exhibit abnormalities in target organs before the onset of autoimmune destruction, which may trigger leukocyte infiltration. These abnormalities may result from immune cell deficiencies, particularly in macrophages. Furthermore, NOD mice show altered phosphorylation of cellular factors, which can disturb the equilibrium of O-linked glycosylation and phosphorylation.
NOD mice also respond differently to glucose tolerance tests compared to other mouse strains. For example, 6-week-old NOD/scid mice exhibited a blunted early rise in blood glucose levels during i.p. glucose tolerance tests but normalized their blood glucose levels at a similar rate as other strains. NOD/scid mice also showed a faster and larger overall insulin release during these tests, indicating that they are more insulin-resistant than B6/scid mice.
The incidence of diabetes in NOD mice is influenced by environmental factors such as housing conditions, health status, and diet. For instance, NOD mice maintained in sterile environments will develop spontaneous diabetes. The incidence of spontaneous diabetes also varies between female and male NOD mice, with a higher incidence observed in females.
In summary, NOD mice exhibit insulin resistance and are a valuable model for studying the development and treatment of autoimmune insulin-dependent diabetes.
California's Red Light Laws: What You Need to Know
You may want to see also

Glucose tolerance tests
In the context of NOD mice, glucose tolerance tests are used to study the development of diabetes and the underlying genetic and physiological mechanisms. NOD mice are a widely used animal model for type 1 diabetes, as they spontaneously develop autoimmune diabetes that shares many similarities with human type 1 diabetes. This makes them a valuable tool for understanding the disease and testing potential treatments.
In addition to standard glucose tolerance tests, researchers may also perform insulin tolerance tests, in which insulin is injected, and blood glucose levels are monitored to assess how effectively the body can lower blood glucose levels in response to insulin. This can provide insights into insulin resistance, which is a key feature of type 2 diabetes.
Executive Leadership: Chief's Role and Responsibilities
You may want to see also

Hyperglycaemia and insulitis
NOD mice are a widely used animal model for Type 1 Diabetes (T1D) and have been used to study the interface between type 1 and type 2 diabetes. They are insulin-resistant to some degree, and this has been linked to the production of inflammatory cytokines such as IL-1 in the insulitic islets.
Insulitis is a condition characterised by leukocytic infiltration of the pancreatic islets, which results in the destruction of insulin-secreting β-cells. This destruction is believed to be mediated by T lymphocytes, though the direct role of B lymphocytes is still unclear. Insulitis and the resulting diabetes can occur even in the absence of functional B cells, as demonstrated by studies using B-cell deficient NOD mice.
In NOD mice, diabetes develops spontaneously, and the onset of diabetes is characterised by mild glycosuria (glucose in urine) and non-fasting hyperglycaemia. The incidence of disease onset is impacted by sex, with more females than males developing spontaneous diabetes by 30 weeks of age. The onset of diabetes occurs earlier in females, with a median incidence at 18 weeks, and a marked decrease in insulin content observed at 12 weeks of age.
Hyperglycaemia is a key feature of diabetes and is characterised by high blood glucose levels. In NOD mice, hyperglycaemia can occur suddenly, with normal glucose values followed by acute hyperglycaemia, or it can be progressive, with a gradual increase in blood glucose levels over time. The development of hyperglycaemia in NOD mice has been linked to a decrease in β-cell proliferative capacity and changes in islet architecture, leading to a reduction in the β-cell population.
In summary, hyperglycaemia and insulitis are closely related in the context of NOD mice. Insulitis leads to the destruction of β-cells, which are responsible for insulin secretion and glucose regulation. This disruption results in hyperglycaemia, characterised by elevated blood glucose levels, which can have acute or progressive onset. The incidence and progression of hyperglycaemia and diabetes in NOD mice are influenced by genetic, environmental, and sex-related factors, making them a valuable model for studying the complex pathophysiology of diabetes.
Pennsylvania and Constitution: What's the Difference?
You may want to see also
Explore related products
$70

Genetic loci and susceptibility
The non-obese diabetic (NOD) mouse is a widely recognized model for studying type 1 diabetes, exhibiting a strong genetic susceptibility to the disease. This susceptibility is influenced by various genetic loci, providing valuable insights into the pathogenesis of diabetes.
One of the critical genetic loci associated with susceptibility to insulin-dependent diabetes mellitus (IDDM) in NOD mice is the idd1 locus, which corresponds to the major histocompatibility complex (MHC) class II I-Ag7. The MHC locus is a well-established susceptibility factor for autoimmune diabetes in both mice and humans, emphasizing its significance in disease development.
Additionally, the Idd3 locus plays a crucial role in NOD mice's susceptibility to autoimmune diseases. Variants in this locus, specifically IL-2 variants, can alter the function and development of Treg cells. IL-2 is a key cytokine that promotes either immunity or tolerance, depending on its concentration. In NOD mice, low levels of IL-2 may contribute to the breakdown of immune tolerance and the development of autoimmunity by impacting the survival of Treg cells.
Another important consideration is the role of the CTLA-4 gene. NOD mice have a mutation in exon 2 of this gene, resulting in incorrect splicing. CTLA-4 is essential for suppressing the T-cell immune response. When it malfunctions, T-cells can attack insulin-producing cells, leading to the destruction of pancreatic β cells and the onset of diabetes.
Furthermore, the introduction of diabetes resistance loci in NOD.CD86-/- mice has generated congenic strains that are completely protected from both autoimmune diabetes and neuropathy. These strains, NOD.CD86-/–Idd3/5 and NOD.CD86-/–Idd3/10/18, offer valuable insights into the genetic factors and mechanisms driving the development of these autoimmune conditions.
In conclusion, the genetic susceptibility of NOD mice to diabetic glucose intolerance is a complex interplay of various genetic loci. These loci, including idd1, Idd3, and CTLA-4, influence the function of immune cells, cytokine production, and the development of autoimmunity. By studying these loci and their interactions, researchers gain valuable insights into the pathogenesis of diabetes and explore potential therapeutic interventions.
Political Parties: Are They Constitutional?
You may want to see also

Pancreatic pathology
Non-obese diabetic (NOD) mice are the most commonly used animal model for studying diabetes because they spontaneously develop type 1 diabetes (T1D) and share similarities with the human disease. NOD mice are highly susceptible to pancreatic autoimmunity, which can lead to the development of autoimmune diabetes and delayed growth of pancreatic cancer.
The onset of diabetes in NOD mice is largely mediated by autoreactive T cells, which target and destroy the pancreatic β-cells. This results in a decrease in insulin levels and hyperglycemia. The progression of diabetes correlates with the extent of inflammation of the pancreatic islets and the loss of β-cell mass.
Histological analysis of NOD mice has shown that the immune infiltrate begins to surround the pancreatic islets at about 4–5 weeks of age, a condition known as peri-insulitis. After about 10 weeks, immune cells can be found within the pancreatic islets, a stage called insulitis. The inflammatory infiltrate consists initially of dendritic cells and macrophages, with lymphocytes becoming the predominant cellular type over time.
In terms of pancreatic pathology, NOD mice exhibit similarities to human type 1 diabetes, with abnormalities in target organs before the onset of autoimmune destruction. However, it is important to note that a small percentage of NOD mice do not develop overt diabetes even after 28–35 weeks of age, and the progression of pancreatic inflammation has been observed to occur independently of diabetes onset.
Additionally, when comparing the onset of diabetes in NOD mice, studies have shown that there are two distinct pathways: acute and progressive. The acute onset is characterised by sudden symptomatic onset and extensive β-cell ablation, while the progressive onset involves a gradual impairment of glycemic regulation. These differences in disease onset may be associated with variations in pancreatic pathology, such as immunophenotype and β-cell mass, highlighting the need for further longitudinal studies to validate and understand the underlying metabolic differences.
The Quartering Act: Constitutional Rights and Wrongs
You may want to see also
Frequently asked questions
The Non-Obese Diabetic (NOD) mouse strain is an animal model for type 1 diabetes that spontaneously develops autoimmune diabetes.
Diabetes in NOD mice is characterised by hyperglycaemia and insulitis, a leukocytic infiltration of the pancreatic islets. The onset of diabetes is associated with glycosuria and non-fasting hyperglycaemia.
Glucose tolerance tests involve challenging NOD mice with varying doses of glucose and monitoring their blood glucose and serum insulin concentration over time.