Urinary incontinence is a common condition, affecting 1 in 4 Australian adults, where the patient experiences a lack of control over their bladder. It is often associated with prostate disease, with 30% of men aged 70-84 and 50% of men over 85 experiencing urge incontinence. Prostate surgery can cause incontinence, with patients reporting the use of diapers and pads post-surgery. However, there are surgical techniques aimed at preserving continence after radical retropubic prostatectomy (RRP), with studies showing that modified RRP can achieve significantly better continence rates at discharge, 1 month, and 3 months post-surgery.
Explore related products
$9.99
What You'll Learn

Continence rates after RRP
According to a study by Phillip M Pierorazio et al., preoperative risk stratification can predict the likelihood of achieving concurrent PSA-free survival, continence, and potency after RRP. The study analysed 416 patients and found that low-risk patients had a higher chance of remaining disease-free, continent, and potent after surgery compared to intermediate and high-risk patients. Specifically, the continence rates for low-risk, intermediate-risk, and high-risk patients at a median follow-up of 4.4, 4.8, and 7.1 years were 93.8%, 94.4%, and 93.3%, respectively.
Another study compared modified RRP (group 1: 250 patients) with unmodified RRP (group 2: 50 patients) and found that the modified approach significantly improved continence rates. At discharge, 62.4% of group 1 patients achieved continence compared to 14.0% in group 2. At 1 month, the rates were 74.0% and 30%, respectively, and at 3 months, they were 85.2% and 46%. However, long-term recovery rates were similar between the two groups, with 94% in group 1 and 90% in group 2 achieving continence.
Several surgical techniques have been proposed to optimize early urinary continence recovery after RRP. These include minimizing damage to the internal and external urinary sphincters, maximizing urethral length sparing, creating a secure vesicourethral anastomosis, and providing anterior and posterior myo-fascio-ligamentous support to the anastomosis. Additionally, studies have suggested that modifications to the posterior reconstruction of the rhabdosphincter can significantly reduce the time to continence without adverse effects.
Overall, while continence rates after RRP can vary, surgical techniques and preoperative risk assessments play a crucial role in optimizing outcomes and helping patients regain urinary control as quickly as possible.
Exploring the National Constitution Center: A Time-Bound Guide
You may want to see also

Surgical techniques to preserve continence
Radical prostatectomy significantly impacts the inherent anatomy of the male pelvis and the functional mechanisms of urinary continence. Urinary incontinence after surgery is the most debilitating complication, affecting patients' quality of life, and may influence their choice of treatment.
There are several surgical techniques that have been demonstrated to support the preservation of continence during robot-assisted radical prostatectomy (RARP). The key goal during RARP is to preserve the inherent anatomy of the male pelvis and the functional mechanisms of urinary continence.
Bladder neck preservation (BNP) is one such approach. It has been associated with significantly better urinary continence outcomes at 3–4 months compared with patients who underwent RARP without BNP. A newer described technique of extended bladder neck sparing is complete urethral preservation, during which the intraprostatic urethra is preserved in cases with no central zone tumours.
Another technique for full functional-length urethra (FFLU) preservation during radical prostatectomy has been described by Schlomm et al. This technique involves a meticulous apical dissection along anatomic landmarks, preserving the length of the intraprostatically located membranous urethra. With this technique, they demonstrated in 691 men that UC rates were 50.1% and 30.9% 1 week after catheter removal for patients with and without the FFLU technique, respectively.
Kaouk et al. have reported excellent continence rates with their technique. The median time using a Foley catheter after surgery was 4 days, 56% of the patients had immediate continence after Foley removal, and the continence rate was 96.7% at 3 months postoperatively.
Other proposed modifications to improve urinary continence include subapical urethral dissection, anterior and posterior reconstruction, and nerve-sparing and Retzius-sparing.
Rebellion Legality: Exploring Constitutional Rights and Limits
You may want to see also

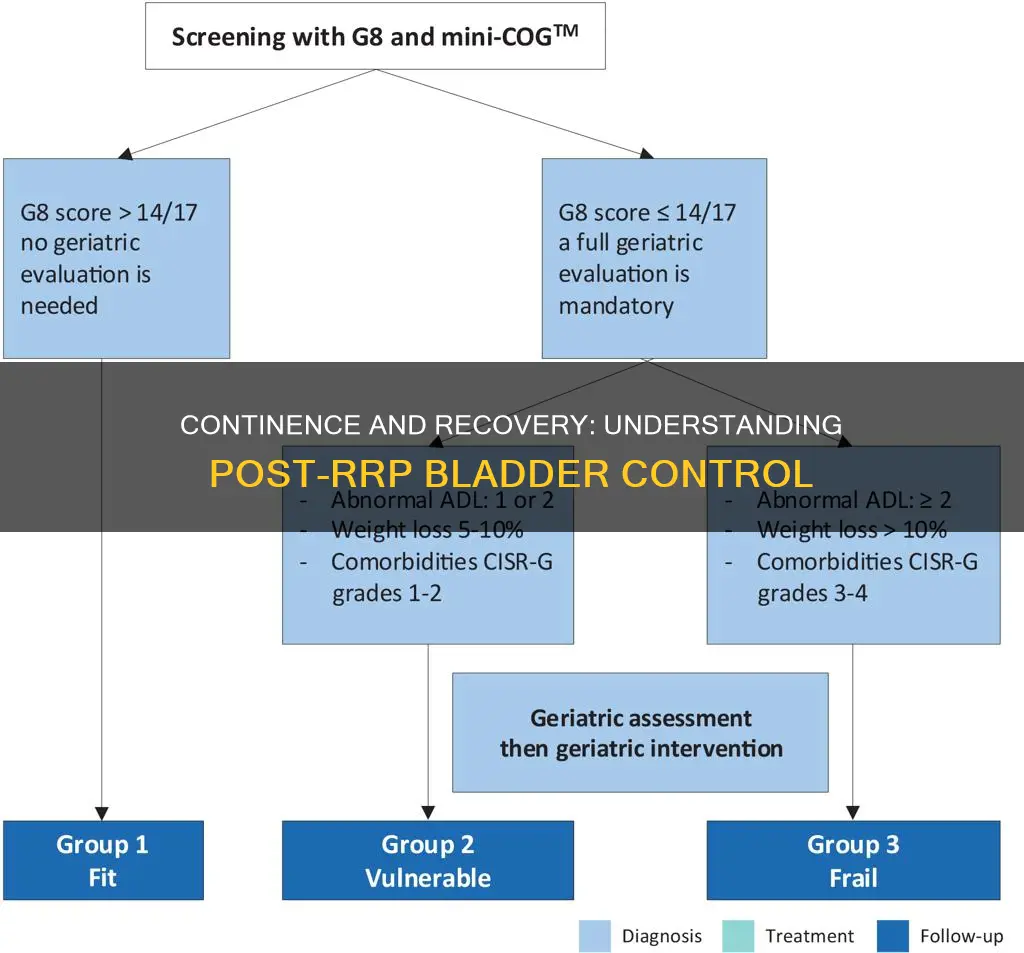
Risk factors for incontinence after RRP
Radical retropubic prostatectomy (RRP) is a surgery used to treat prostate cancer. The two most common complications of RRP are incontinence and impotence. Inguinal hernia (IH) has also emerged as a complication, with an estimated incidence of 15-20% after RRP.
Several risk factors for incontinence after RRP have been identified:
- Age: Older age is associated with delayed continence recovery but not permanent incontinence.
- Posterior urethral length: A shorter posterior urethral length increases the risk of urinary incontinence and delays continence recovery.
- Anastomotic stricture: This was identified as an independent prognostic factor for incontinence.
- Bilateral neurovascular bundle resection: This was found to be a significant risk factor for incontinence.
- Pre-operative risk stratification: Low-risk patients are more likely to remain continent after surgery than higher-risk patients.
It is important to note that the recovery of continence after RRP can take time, with some studies showing improvements in continence rates up to two years after surgery. Additionally, the definition of continence can vary, with some studies defining it as no or occasional pad use, while others define it as using one pad per day.
Key Sources of the UK Constitution
You may want to see also
Explore related products

Early continence recovery after RRP
One study compared modified RRP (250 patients) with unmodified RRP (50 patients) and found that the modified procedure resulted in significantly better continence rates at discharge (62.4% vs. 14.0%), 1 month (74.0% vs. 30%), and 3 months (85.2% vs. 46%). The long-term recovery rates were similar between the two groups (94% vs. 90%). This indicates that technical modifications can significantly reduce the time to achieve continence without adverse effects.
To enhance early continence recovery, surgical techniques should focus on minimising damage to the internal and external urinary sphincters and their neural supply, maximising urethral length preservation, creating a secure vesicourethral anastomosis, and providing anterior and posterior myo-fascio-ligamentous support.
Additionally, preoperative risk stratification plays a vital role in predicting the likelihood of achieving concurrent PSA-free survival, continence, and potency after RRP. Low-risk patients tend to have higher rates of disease-free, continent, and potent outcomes compared to higher-risk patients. Physicians should consider these aggregate outcomes when counselling patients about the potential results of RRP.
Furthermore, specific surgical techniques, such as the dehydrated human amnion/chorion membrane allograft nerve wrap and bladder neck sling suspension, have shown promising results in accelerating early continence recovery and improving potency following robot-assisted radical prostatectomy.
Overall, early continence recovery after RRP is a complex process that requires careful surgical techniques, risk assessments, and patient counselling to optimise outcomes and enhance patients' quality of life.
Presidential Cabinet: Examples and Their Roles
You may want to see also

Impact of RRP on urinary continence
Radical retropubic prostatectomy (RRP) is a common treatment for prostate cancer, which is one of the most prevalent cancers among men in the United States. However, one of the most common concerns following this procedure is urinary incontinence (UI), which can have adverse effects on patients' quality of life, including stigmatization, social isolation, depressive symptoms, loneliness, and embarrassment.
Several factors influence the prevalence of UI after RRP, including preoperative patient characteristics, surgeon experience, surgical technique, and methods used to collect and report data. For example, one study found a correlation between the volume of periurethral fibrosis and the number of postoperative operations for urethral strictures in patients with incontinence. Another study found that patients with higher preoperative prostate-specific antigen levels had a lower likelihood of achieving the "trifecta" of disease-free survival, urinary continence, and sexual potency after RRP.
The rate of UI after RRP varies across studies, with 12-month urinary continence recovery rates ranging from 84% to 97% in some studies and 4% to 31% in others. However, RRP has been found to result in higher occurrences of UI compared to other surgical methods such as robotic-assisted radical prostatectomy (RARP) and laparoscopic radical prostatectomy (LRP). For example, one study found that patients who underwent RARP had better 12-month urinary continence recovery compared to those who underwent RRP.
While there is a risk of UI after RRP, it is important to note that individual experiences may vary. Some patients may regain full control within a few weeks, while others may continue to experience leakage years after the surgery. Additionally, there are management options available, such as penile implants and kegel exercises, that can help improve urinary control.
Key Features of Our Constitution
You may want to see also
Frequently asked questions
RRP stands for Radical Retropubic Prostatectomy, a type of surgery involving the prostate.
The trifecta analysis assesses the likelihood of three outcomes after RRP: disease-free survival, urinary continence, and sexual potency.
Recovery of continence after RRP can be influenced by age, pathologic stage, and Gleason score. Surgical techniques, such as the modified posterior reconstruction of the rhabdosphincter, can also impact recovery.
RRP carries risks of urinary incontinence and sexual dysfunction. The likelihood of these risks varies depending on preoperative risk factors and surgical techniques.
Incontinence after RRP can vary. Some individuals may experience early continence recovery within a few months, while others may still require pads or diapers several years after surgery. Seeking advice from others with similar experiences can provide insights into potential treatments and lifestyle changes.
















![Adult Incontinence Booster Pads Extra Absorbent with Adhesive [Large 3.5''x11.5''] Protection for Men and Women - Soft Disposable Diaper Top Liner Pad - Comfortable 3.5x11.5 inches (24)](https://m.media-amazon.com/images/I/71jq51wCH-L._AC_UL320_.jpg)


























