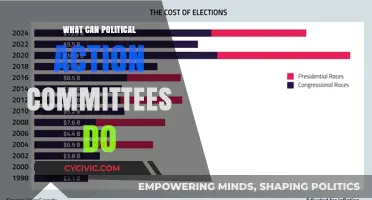
The validity of surgical outcomes can be significantly undermined by political influences that prioritize agendas over patient care. Political interference in healthcare decision-making, such as resource allocation, funding priorities, or policy mandates, can distort surgical practices and compromise patient safety. For instance, politically driven budget cuts may limit access to essential equipment or staffing, while partisan policies might dictate which procedures are covered or prioritized, regardless of medical necessity. Additionally, political favoritism in hospital administration or research funding can skew surgical innovations and data, leading to biased outcomes. These factors collectively erode the integrity of surgical validity, highlighting the need for a depoliticized approach to healthcare to ensure evidence-based, patient-centered practices.
Explore related products
What You'll Learn
- Biased Patient Selection: Excluding certain demographics skews results, undermining surgery's effectiveness across diverse populations
- Conflicts of Interest: Financial ties to medical companies can distort research findings and recommendations
- Data Manipulation: Altering surgical outcomes data to favor specific agendas invalidates scientific integrity
- Policy Influence: Political pressure may prioritize cost over patient safety, compromising surgical standards
- Media Misrepresentation: Sensationalized reporting of surgical risks or benefits misleads public perception and trust

Biased Patient Selection: Excluding certain demographics skews results, undermining surgery's effectiveness across diverse populations
Biased patient selection is a critical issue that can significantly undermine the validity and generalizability of surgical research and outcomes. When certain demographics are systematically excluded from studies or clinical trials, the results may not accurately reflect the surgery's effectiveness across the broader population. This exclusion can occur due to various factors, such as socioeconomic status, race, ethnicity, gender, age, or pre-existing health conditions. For instance, if a study on a new surgical technique primarily includes young, healthy, affluent males, the findings may not be applicable to older adults, women, or individuals from lower socioeconomic backgrounds who often face different health challenges and comorbidities. This skewed representation limits the ability to draw meaningful conclusions about the surgery's efficacy and safety for diverse patient groups.
The consequences of biased patient selection extend beyond research settings, impacting clinical practice and healthcare policy. Surgeons and healthcare providers rely on evidence-based guidelines to make informed decisions about patient care. If the evidence is derived from a non-representative sample, it can lead to inappropriate treatment recommendations for underrepresented populations. For example, a surgical procedure proven effective in a predominantly Caucasian population might not yield the same results in patients of Asian or African descent due to differences in anatomy, physiology, or disease prevalence. This mismatch can result in suboptimal outcomes, increased complications, and diminished trust in the healthcare system among marginalized communities.
Addressing biased patient selection requires a multifaceted approach. Researchers must prioritize inclusivity by designing studies that actively recruit participants from diverse demographic groups. This can involve targeted outreach efforts, community engagement, and the use of inclusive eligibility criteria that do not unnecessarily exclude individuals based on factors like age, weight, or comorbid conditions. Additionally, funding agencies and regulatory bodies should mandate diversity in clinical trials, ensuring that research proposals demonstrate a clear plan for inclusive patient recruitment and retention. By broadening the participant pool, studies can generate more robust and generalizable data, enhancing the validity of surgical interventions across populations.
Transparency and accountability are also essential in mitigating the effects of biased patient selection. Researchers should explicitly report the demographic characteristics of their study populations, including any exclusions and the reasons behind them. Peer reviewers and journal editors play a crucial role in scrutinizing manuscripts to ensure that patient selection biases are identified and addressed. Furthermore, meta-analyses and systematic reviews should critically evaluate the demographic representation across studies to highlight gaps and inform future research priorities. This collective effort can help identify and rectify biases, fostering a more equitable evidence base for surgical practice.
Ultimately, the exclusion of certain demographics in surgical research perpetuates health disparities and limits the advancement of medical knowledge. By acknowledging and addressing biased patient selection, the medical community can ensure that surgical interventions are developed, tested, and implemented in a manner that benefits all patients, regardless of their background. This commitment to inclusivity not only strengthens the scientific validity of research but also aligns with ethical principles of equity and justice in healthcare. Without it, the effectiveness and applicability of surgeries will remain compromised, hindering progress toward better health outcomes for diverse populations.
Engage Locally: A Canadian Guide to Joining Local Politics
You may want to see also

Conflicts of Interest: Financial ties to medical companies can distort research findings and recommendations
Conflicts of interest arising from financial ties to medical companies pose a significant threat to the validity and integrity of surgical research and practice. When surgeons, researchers, or institutions have financial relationships with pharmaceutical firms, medical device manufacturers, or other industry players, their objectivity can be compromised. These ties may manifest through consulting fees, research grants, stock ownership, or royalties, creating a situation where personal financial gain could influence professional decisions. For instance, a surgeon with financial ties to a specific medical device company might be more inclined to recommend or use that company’s products, even if alternatives are more effective or cost-efficient. This bias can distort research findings, clinical guidelines, and patient care, ultimately undermining the trustworthiness of surgical outcomes.
The distortion of research findings is a particularly concerning consequence of such conflicts of interest. Studies have shown that industry-funded research is more likely to produce favorable results for the sponsoring company’s products compared to independently funded studies. In surgery, this could mean overstating the benefits of a particular device, procedure, or medication while downplaying risks or side effects. For example, a trial funded by a manufacturer of a new surgical implant might selectively report positive outcomes or exclude unfavorable data, leading to biased conclusions. Such manipulated findings can misguide other surgeons and healthcare providers, potentially leading to suboptimal patient care and compromised surgical validity.
Recommendations and clinical guidelines are another area vulnerable to the influence of financial conflicts of interest. Surgeons or experts with ties to medical companies may advocate for the use of specific products or procedures in guidelines, even if evidence supporting their superiority is weak. This can result in the widespread adoption of less effective or more expensive interventions, driven by financial incentives rather than patient needs. For instance, a guideline committee member with financial ties to a robotic surgery system manufacturer might push for its inclusion as a first-line treatment, despite limited evidence of its benefits over traditional methods. Such biased recommendations erode the credibility of surgical guidelines and harm patient outcomes.
Transparency and disclosure are critical in mitigating the impact of financial conflicts of interest, but they are often insufficient on their own. While disclosing ties to medical companies is a step toward accountability, it does not eliminate the potential for bias. Institutions and regulatory bodies must implement stricter policies, such as limiting the involvement of conflicted individuals in research or guideline development, or requiring independent review of industry-funded studies. Additionally, surgeons and researchers must prioritize ethical considerations over financial gain, ensuring that their decisions are based on robust evidence and patient welfare rather than personal profit.
Ultimately, the presence of financial conflicts of interest in surgery not only jeopardizes the validity of research and recommendations but also erodes public trust in the medical profession. Patients rely on surgeons and researchers to provide unbiased, evidence-based care, and any perception of industry influence can undermine this trust. Addressing these conflicts requires a multifaceted approach, including increased scrutiny, stronger regulations, and a cultural shift toward prioritizing patient interests above financial incentives. By doing so, the surgical community can uphold the integrity of its practices and ensure that patient care remains the paramount concern.
Canada's Political Stability: A Comprehensive Analysis of Current Dynamics
You may want to see also

Data Manipulation: Altering surgical outcomes data to favor specific agendas invalidates scientific integrity
Data manipulation in the context of surgical outcomes is a grave issue that directly undermines the credibility and reliability of medical research. When surgical data is altered to favor specific agendas, whether political, financial, or institutional, it distorts the scientific record and misleads both the medical community and the public. Such manipulation can involve fabricating results, selectively reporting positive outcomes, or omitting unfavorable data to align with predetermined conclusions. This practice not only invalidates the integrity of individual studies but also erodes trust in the broader field of surgery and medical science. For instance, if a study claims a new surgical technique has a 95% success rate but excludes cases where complications occurred, the findings become misleading and potentially dangerous for patients.
The consequences of data manipulation extend beyond academic dishonesty; they directly impact patient care and safety. Surgeons and healthcare providers rely on accurate data to make informed decisions about treatment options. If the data is manipulated, they may adopt procedures or techniques that are less effective or even harmful. For example, a politically motivated study might promote a cost-effective surgical method without disclosing its higher risk of complications, leading to suboptimal patient outcomes. This not only jeopardizes individual health but also wastes healthcare resources and undermines public confidence in medical institutions.
Political agendas often drive data manipulation in surgical research, particularly when funding, policy decisions, or institutional reputations are at stake. Governments, pharmaceutical companies, or medical device manufacturers may pressure researchers to skew results to support their interests. For instance, a government might fund a study to demonstrate the success of a public health initiative, leading researchers to inflate positive outcomes. Similarly, a company might sponsor research to promote a new surgical device, incentivizing investigators to downplay its limitations. Such conflicts of interest corrupt the scientific process and prioritize political or financial gains over patient well-being.
Preventing data manipulation requires robust oversight, transparency, and adherence to ethical standards. Peer review processes must be rigorous, and journals should demand raw data and detailed methodologies to verify findings. Institutions and funding bodies must enforce strict guidelines to mitigate conflicts of interest and ensure researchers act with integrity. Additionally, whistleblowing mechanisms should be established to allow reporting of unethical practices without fear of retaliation. By fostering a culture of accountability and transparency, the medical community can safeguard the validity of surgical research and maintain public trust.
Ultimately, data manipulation in surgical outcomes is a betrayal of the core principles of science and medicine. It not only distorts knowledge but also endangers lives by promoting flawed practices. Addressing this issue demands collective action from researchers, institutions, and policymakers to uphold ethical standards and prioritize patient welfare above all else. Only through unwavering commitment to truth and transparency can the integrity of surgical research be preserved in the face of political and external pressures.
Seeking Safety: A Guide to Canadian Asylum for Pakistanis
You may want to see also
Explore related products

Policy Influence: Political pressure may prioritize cost over patient safety, compromising surgical standards
Political pressure on healthcare policies often stems from the need to allocate limited resources efficiently, but this can lead to a dangerous prioritization of cost-cutting over patient safety. When governments or healthcare administrators face budgetary constraints, they may implement policies that reduce surgical funding, limit access to advanced medical technologies, or shorten hospital stays to save money. While these measures may appear fiscally responsible, they can directly compromise the validity and safety of surgical procedures. For instance, underfunded hospitals may be forced to use outdated equipment or hire less experienced staff, increasing the risk of surgical errors and complications. This erosion of standards undermines the very foundation of surgical validity, as patient outcomes become secondary to financial considerations.
One of the most direct ways political pressure can influence surgery validity is through the imposition of cost-containment policies that restrict access to necessary resources. For example, policies may cap the number of surgeries a hospital can perform or limit the use of expensive but essential materials like implants or specialized instruments. Such restrictions can force surgeons to make difficult decisions, potentially opting for less effective but cheaper alternatives. This not only jeopardizes the success of individual surgeries but also erodes public trust in the healthcare system. When political agendas dictate clinical decisions, the integrity of surgical practice is compromised, and patients may suffer as a result.
Moreover, political pressure often leads to the implementation of performance metrics that prioritize efficiency over quality. Hospitals and surgeons may be incentivized to reduce procedure times or increase the volume of surgeries performed, regardless of whether these practices align with best patient care. For example, policies that penalize longer hospital stays can push providers to discharge patients prematurely, increasing the likelihood of post-surgical complications. These metrics, driven by political and economic goals, can create a culture where speed and cost-effectiveness overshadow the meticulous care required for successful surgical outcomes.
Another critical issue arises when political influence leads to inadequate investment in surgical training and education. Budget cuts to medical education programs can result in a shortage of skilled surgeons and support staff, leaving healthcare systems ill-equipped to handle complex procedures. Additionally, reduced funding for continuing education limits surgeons' ability to stay updated with the latest techniques and technologies, further compromising surgical standards. When political decisions prioritize short-term financial gains over long-term investments in healthcare infrastructure, the validity and safety of surgeries are inevitably undermined.
Finally, political pressure can exacerbate disparities in access to quality surgical care, particularly in underserved or rural areas. Policies that allocate resources disproportionately to urban or politically favored regions can leave marginalized populations with substandard surgical options. This not only perpetuates health inequities but also diminishes the overall validity of surgical practices by creating a two-tiered system where patient safety is contingent on geographic or socioeconomic status. To preserve the integrity of surgery, policymakers must recognize that patient safety and surgical standards are non-negotiable, even in the face of budgetary constraints. Balancing fiscal responsibility with a commitment to high-quality care is essential to ensuring that political influence does not ruin the validity of surgical procedures.
Church and Politics: Navigating Faith's Role in Societal Advocacy
You may want to see also

Media Misrepresentation: Sensationalized reporting of surgical risks or benefits misleads public perception and trust
Media misrepresentation, particularly through sensationalized reporting, poses a significant threat to the validity of surgical practices by distorting public perception and eroding trust. When media outlets prioritize dramatic headlines over factual accuracy, they often exaggerate surgical risks or overpromise benefits, creating a skewed narrative that misleads the public. For instance, a minor complication rate might be portrayed as a widespread danger, or a procedure’s limited success might be hyped as a miracle cure. Such distortions not only misinform patients but also fuel unwarranted fears or unrealistic expectations, undermining the credibility of surgical interventions.
Sensationalized reporting often stems from the media’s reliance on attention-grabbing stories to drive viewership or readership. In the process, nuanced medical information is oversimplified or taken out of context, leading to misinterpretation. For example, a study highlighting rare side effects of a surgery might be framed as a warning against the procedure altogether, ignoring its overall safety and efficacy. This kind of reporting ignores the complexity of surgical decision-making, which involves weighing individualized risks and benefits, and instead presents a one-sided, often alarming perspective that can deter patients from seeking necessary care.
The impact of such media misrepresentation extends beyond individual patients to influence public policy and healthcare discourse. When sensationalized stories go viral, they can shape political agendas and public opinion, potentially leading to misguided regulations or funding decisions. For instance, a single high-profile case of surgical complication, amplified by media hype, could spark calls for restrictive measures on a procedure, even if the overall data supports its safety and effectiveness. This politicization of surgery based on misrepresented information can hinder medical progress and limit patient access to beneficial treatments.
Moreover, media misrepresentation damages the trust between patients and healthcare providers. When patients encounter conflicting or exaggerated information, they may question the motives of surgeons or the healthcare system as a whole. This distrust can lead to hesitancy in accepting surgical recommendations, even when they are evidence-based and in the patient’s best interest. Rebuilding this trust requires transparent communication from medical professionals and a commitment from media outlets to report on surgical outcomes responsibly, balancing accuracy with accessibility.
To mitigate the effects of media misrepresentation, stakeholders must collaborate to promote accurate and balanced reporting. Medical professionals can play a proactive role by engaging with journalists to provide context and clarify complex surgical data. Media organizations, in turn, should adhere to ethical standards that prioritize factual reporting over sensationalism. Public education campaigns can also empower individuals to critically evaluate medical news, encouraging them to seek information from reliable sources. By addressing the root causes of sensationalized reporting, it is possible to restore public confidence in surgery and safeguard its validity in the face of political and social influences.
Empowering Change: How Politics Shapes Society and Drives Progress
You may want to see also
Frequently asked questions
Political interference can compromise surgery validity by imposing non-medical criteria for procedures, such as restricting access based on political agendas rather than clinical need, or prioritizing certain demographics over others for resource allocation.
Funding politics can ruin surgery validity by limiting access to necessary resources, cutting budgets for essential equipment or staff, or diverting funds to politically favored areas, leading to suboptimal patient care and increased surgical risks.
Yes, political polarization can erode ethical standards by promoting policies that prioritize political gain over patient welfare, such as pressuring surgeons to perform unnecessary procedures or restricting evidence-based practices due to ideological opposition.
Politicization of medical research can undermine surgery validity by suppressing or manipulating data to align with political narratives, leading to flawed surgical techniques, inadequate safety protocols, or the adoption of unproven methods.