Frailty is a state of increased vulnerability to poor resolution of homeostasis following stress and is a consequence of a cumulative decline in multiple physiological systems over a lifespan. It is not an inevitable part of aging, but the risk of frailty increases with age and the incidence of diseases. While frailty is a leading cause of death in older people, it is often not recognized nor considered at the end of life. This late recognition can impede patient-centred decisions and lead to inappropriate life-saving interventions. However, severe frailty is an end-of-life state and should trigger healthcare professionals to discuss end-of-life needs and preferences.
| Characteristics | Values |
|---|---|
| Definition | Frailty syndrome is defined as age-related deficits in normal function and involving several body systems. |
| Diagnosis | There is no universal diagnostic criterion for frailty. Diagnosis is based on a combination of signs and symptoms. |
| Criteria | Weakness, slowness, low level of physical activity, easy exhaustion, poor endurance, and loss of weight. |
| Prevalence | Frailty is estimated to range from 12% to 24% in people over 50. |
| Risk Factors | Age, malnutrition, multiple long-term health conditions, cognitive impairment, diabetes, obesity, depression, loneliness, smoking, sedentary lifestyle, low level of physical exercise, etc. |
| Prevention/Treatment | Regular physical activity, healthy diet, prudent financial planning, and social engagement. |
| Identification | Comprehensive Geriatric Assessment (CGA) is a useful tool to identify end-of-life needs and direct care plans for the frail elderly. |
| Outcome | Frailty predicts increased falls, hospitalization, and mortality. |
Explore related products
What You'll Learn

Frailty is a leading cause of death in older people
Frailty is a state of vulnerability to poor resolution of homeostasis following a stressor. It is a consequence of the cumulative decline in multiple physiological systems over a lifespan. This cumulative decline erodes homeostatic reserve, and relatively minor stressors can trigger disproportionate changes in health status, such as a fall or delirium. Frailty is associated with an increased risk of developing delirium and subsequent reduced survival.
The unpredictable nature of the decline in frailty makes it difficult to know when someone is nearing the end of their life. Healthcare professionals may be reluctant to identify frailty as indicative of end-of-life when there is no clear underlying pathology. However, the identification of end-of-life is important as it allows for an optimal clinical response and gives the older person and their family a sense of security and control.
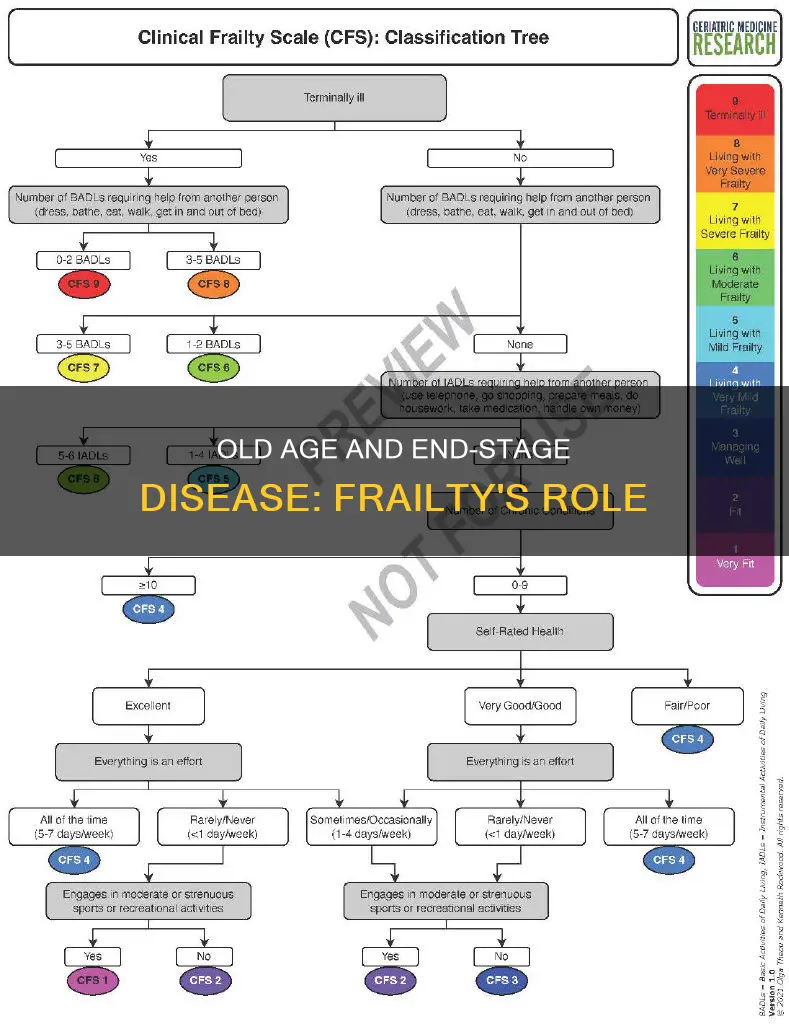
There are several tools to help identify people nearing the end of their life, such as the Comprehensive Geriatric Assessment (CGA), which can be used to identify needs and direct a focused care plan. Additionally, the Edmonton Frail Scale is a quick and valid assessment tool that can be used by non-geriatricians to identify frailty.
The prevention and treatment of frailty include regular exercise, a balanced diet, and the prevention of socioeconomic and environmental stress. When diagnosed with frailty, a team-based approach involving a geriatric physician, nurse, social worker, and therapists has proven invaluable in improving a patient's status.
The Constitution's Democracy Mentions: A Comprehensive Count
You may want to see also

Frailty is not an inevitable part of ageing
While ageing is an inevitable part of the life course, frailty is not an inevitable consequence of ageing. Frailty is a dynamic medical condition that is characterised by a loss of reserve across multiple parts of the body. It is a state of vulnerability to poor resolution of homeostasis following a stressor event, such as a fall, a urinary infection, or hospitalisation. The onset of frailty can be earlier or delayed, depending on the medical condition of the individual.
Frailty is generally characterised by several physical symptoms, including weakness, slow walking speed, exhaustion, unintentional weight loss, and low activity levels. Lower bone density and osteoporosis are also associated with frailty, increasing the risk of falls and fractures. The greatest common denominator of frailty is muscle loss and a slowing of gait.
Social isolation and loneliness can contribute to the progression of frailty. Additionally, "polypharmacy", or being prescribed five or more medications, is associated with an increased risk of frailty. The presence of frailty can also interfere with how the body absorbs medicines.
There are several strategies to prevent and treat frailty. The first and most important preventive strategy is to exercise regularly, including resistance training, to target major muscle groups. A second strategy is diet; it is important to eat a balanced, protein-rich diet with plenty of fruit and vegetables for the prevention and treatment of frailty. A third strategy is the prevention of socioeconomic and environmental stress through prudent financial planning and social engagement.
Understanding Company Constitution: A Legal Requirement?
You may want to see also

Frailty increases morbidity and mortality when stressed
Frailty is a complex condition that affects multiple organ systems, including the brain, endocrine system, immune system, and skeletal muscle. It is characterised by a decline in physiological reserve, leading to increased vulnerability to stress and adverse health outcomes. This vulnerability is further exacerbated by stressful events, which can trigger disproportionate changes in health status, such as falls or delirium.
Several factors contribute to the progression of frailty, including nutritional deficiencies, sedentary behaviour, stressful living, and the presence of chronic diseases such as cancer, arthritis, heart disease, and diabetes mellitus. The risk of frailty is also influenced by lifestyle choices, with obesity, smoking, and high waist-hip ratios being significant risk factors. Additionally, hormonal changes associated with ageing, such as decreased testosterone in men and estrogen in women, can lead to a decline in muscle mass, contributing to frailty.
The impact of frailty on morbidity and mortality is significant, particularly when individuals undergo surgical procedures or experience new major diseases. Frail patients undergoing oncological liver resections, for example, have demonstrated higher rates of morbidity, major complications, and postoperative liver failure. They also exhibit higher mortality rates and readmission rates. Similarly, frailty increases the risk of morbidity and mortality in patients with cardiovascular disease, and those with diabetes mellitus.
The identification of frailty is crucial for optimising clinical responses and ensuring older individuals receive appropriate care. Tools such as the Edmonton Frail Scale and the Comprehensive Geriatric Assessment (CGA) are valuable in assessing frailty and identifying end-of-life needs. However, late recognition of frailty can impede patient-centred decisions and lead to inappropriate life-saving interventions. Therefore, early identification and intervention are essential to improve outcomes and quality of life for individuals experiencing frailty.
To mitigate the impact of frailty, preventive strategies are crucial. Regular exercise that targets major muscle groups, such as weight lifting, push-ups, and sit-ups, can help delay the onset of frailty and improve muscle strength. Additionally, maintaining a balanced diet and addressing socioeconomic and environmental stressors through financial planning and social engagement can also reduce the progression of frailty. By implementing these strategies, individuals can improve their overall health and potentially delay the onset of frailty-related complications.
Stay-at-Home Orders: Michigan's Constitutional Conundrum
You may want to see also
Explore related products

Frailty is associated with adverse health outcomes
Frailty is a growing global health concern, with major implications for clinical practice and public health. It is a state of vulnerability to poor resolution of homeostasis following stress and is a consequence of a cumulative decline in multiple physiological systems over a lifespan. This decline erodes homeostatic reserve, increasing the risk of adverse outcomes, including falls, delirium, disability, hospitalisation, institutionalisation, and death.
Several factors influence the onset and progression of frailty, including sociodemographic, clinical, lifestyle-related, and biological factors. Ageing, female sex, an unhealthy lifestyle, and lower economic status are identified as potential risk factors. Social factors such as marital status, smoking history, social isolation, and lower levels of education also contribute to the risk of frailty. Additionally, the presence of multiple comorbidities, including diabetes mellitus, respiratory disease, stroke, dementia, and osteoarthritis, is associated with higher documented frailty rates.
The identification and management of frailty are crucial in optimising health outcomes. Frailty assessment tools, such as the Edmonton Frail Scale and the Comprehensive Geriatric Assessment (CGA), are available to help identify and manage frailty in older adults. The management of frail patients should be individualised and tailored to their goals of care and life expectancy. Exercise, diet, and socioeconomic and environmental stress prevention are essential strategies for preventing and treating frailty.
Who Has a Hard Copy of Oregon's Constitution?
You may want to see also

Frailty is a state of vulnerability to poor resolution of homeostasis
Frailty is a complex condition that is often associated with ageing, and it is characterised by increased vulnerability and a reduced ability to maintain homeostasis when exposed to stress. It is a state that arises from the cumulative decline of multiple physiological systems over a person's lifespan, resulting in a decreased ability to recover from minor stressors. This vulnerability to poor resolution of homeostasis can lead to adverse health outcomes and an increased risk of mortality.
The development of frailty is influenced by various factors, including age-related biological changes, cellular damage, and molecular mechanisms. The brain, endocrine system, immune system, and skeletal muscle are among the organ systems most commonly implicated in the progression of frailty. The loss of physiological reserve in these systems contributes to the overall decline associated with frailty. Additionally, physical activity levels and nutritional factors play a role in the onset of frailty, with regular exercise and a balanced diet being protective factors.
The clinical presentation of frailty is distinct and is often characterised by a combination of symptoms, including decreased muscle mass and strength, weight loss, reduced endurance, and decreased physical activity. This collection of symptoms is referred to as the "frailty syndrome" and can be assessed using tools such as the Edmonton Frail Scale and the Comprehensive Geriatric Assessment (CGA). These assessments help identify older individuals who may be approaching the end of their lives and enable healthcare professionals to provide appropriate care and support.
The identification of frailty is crucial, as it allows for informed decision-making regarding invasive procedures or medications. It also helps older individuals and their families prepare for end-of-life care and ensures a sense of security and control. However, frailty is often underrecognised, which can lead to inappropriate interventions and a negative impact on the quality of end-of-life care. Therefore, early and accurate detection of frailty is essential to ensure optimal care and quality of life for older individuals.
In conclusion, frailty is a state of increased vulnerability to poor resolution of homeostasis following exposure to stress. It is a consequence of the cumulative decline of multiple physiological systems, resulting in a decreased ability to maintain homeostasis and an increased risk of adverse health outcomes. The identification and management of frailty are essential to providing appropriate care and improving outcomes for older individuals.
The US Constitution: Foundation of a Nation's Laws and Values
You may want to see also
Frequently asked questions
Frailty syndrome is a combination of age-related deficits in normal function, involving several body systems. It is not a specific disease but a collection of symptoms that can lead to a diagnosis. The symptoms include muscle weakness, slower walking speed, exhaustion, unintentional weight loss, and frequent falls.
Frailty syndrome is caused by a decline in multiple physiological systems, including the brain, endocrine system, immune system, and skeletal muscle. This decline can be influenced by physical activity, nutritional factors, and socioeconomic and environmental stress. Aging, lower levels of DHEA, testosterone, IGF-1, and increased levels of cortisol are also thought to contribute to frailty syndrome.
There is no universal diagnostic criterion for frailty syndrome, but some clinical screening tools are commonly used to identify it. These include the Fried Frailty Phenotype and a deficit accumulation frailty index. The Comprehensive Geriatric Assessment (CGA) is another tool that can be used to identify end-of-life needs and direct a focused care plan.
Frailty is a leading cause of death in older people and is associated with increased morbidity and mortality. It is a state of vulnerability to poor resolution of homeostasis following stress. However, frailty itself is not an inevitable part of aging, and its progress can be slowed or prevented through regular physical activity and a healthy diet.









![Public policy and the frail elderly : a staff report, December 1978. 1979 [Leather Bound]](https://m.media-amazon.com/images/I/61IX47b4r9L._AC_UY218_.jpg)