The question of whether bone spurs are political may seem unusual at first glance, but it intersects with broader societal and historical contexts. Bone spurs, a common medical condition involving bony projections along joints, gained political notoriety during the Vietnam War era when they were cited as a reason for draft deferments, most famously in the case of Donald Trump. This connection has since sparked debates about privilege, inequality, and the ways in which health issues can be weaponized or exploited in political discourse. While bone spurs themselves are apolitical, their role in historical events and their association with controversies highlight how medical conditions can become entangled with political narratives, raising questions about fairness, accountability, and the intersection of health and power.
Explore related products
What You'll Learn
- Healthcare Policy Impact: How bone spur treatments are influenced by government healthcare policies and funding decisions
- Military Exemptions: Bone spurs as a controversial medical exemption from military service in political contexts
- Aging Population: Political debates on managing bone spurs in elderly populations amid rising healthcare costs
- Workplace Regulations: Political discussions on workplace safety laws and bone spur-related disability claims
- Insurance Coverage: Political battles over insurance coverage for bone spur diagnosis, treatment, and surgery

Healthcare Policy Impact: How bone spur treatments are influenced by government healthcare policies and funding decisions
Bone spurs, or osteophytes, are bony projections that develop along joint margins, often causing pain and limiting mobility. While they may seem like a straightforward medical issue, the treatment and management of bone spurs are deeply intertwined with healthcare policies and funding decisions. For instance, in countries with universal healthcare, access to diagnostic tools like X-rays and MRI scans is more equitable, enabling earlier detection and intervention. Conversely, in systems reliant on private insurance, coverage gaps can delay treatment, exacerbating symptoms and increasing long-term costs. This disparity highlights how policy choices directly impact patient outcomes.
Consider the role of funding in determining treatment options. Non-surgical interventions, such as physical therapy and anti-inflammatory medications (e.g., ibuprofen 600 mg, 3 times daily for adults), are often first-line treatments. However, government-funded programs may limit the number of physical therapy sessions covered, forcing patients to pay out-of-pocket or forgo care. Similarly, policies governing prescription drug pricing can make medications like COX-2 inhibitors (e.g., celecoxib 200 mg daily) unaffordable for some. In contrast, systems with robust public funding for preventive care may prioritize early intervention, reducing the need for costly surgeries like spinal decompression or joint replacement.
The political nature of healthcare funding also influences research and innovation. Bone spur treatments, such as shockwave therapy or regenerative medicine (e.g., platelet-rich plasma injections), are often classified as experimental and excluded from insurance coverage. Government investment in clinical trials and evidence-based research could accelerate the adoption of these therapies, but budgetary priorities frequently sideline such initiatives. For example, in the U.S., Medicare’s coverage determinations can set industry standards, yet decisions are often driven by cost containment rather than patient-centered outcomes. This underscores how political agendas shape the availability of cutting-edge treatments.
A comparative analysis of healthcare systems reveals further insights. In Canada, where healthcare is publicly funded, wait times for orthopedic consultations can be lengthy, delaying bone spur treatment. Meanwhile, in Germany’s multi-payer system, patients have greater flexibility in choosing providers but may face higher out-of-pocket costs for specialized care. These examples illustrate how policy frameworks—whether single-payer, multi-payer, or hybrid—dictate the accessibility and quality of care. Policymakers must balance fiscal responsibility with the need to ensure equitable, effective treatment options for conditions like bone spurs.
Ultimately, the politicization of healthcare funding has tangible consequences for bone spur patients. From diagnostic delays to treatment limitations, policy decisions ripple through every stage of care. Advocates and clinicians must push for evidence-based policies that prioritize patient needs, such as expanding coverage for preventive services and investing in research. Practical steps include lobbying for legislative changes, educating patients about their rights, and leveraging data to demonstrate the cost-effectiveness of early intervention. By addressing these systemic issues, we can transform bone spur treatment from a political battleground into a model of accessible, high-quality care.
Mastering Polite Email Requests: Tips for Professional and Courteous Communication
You may want to see also

Military Exemptions: Bone spurs as a controversial medical exemption from military service in political contexts
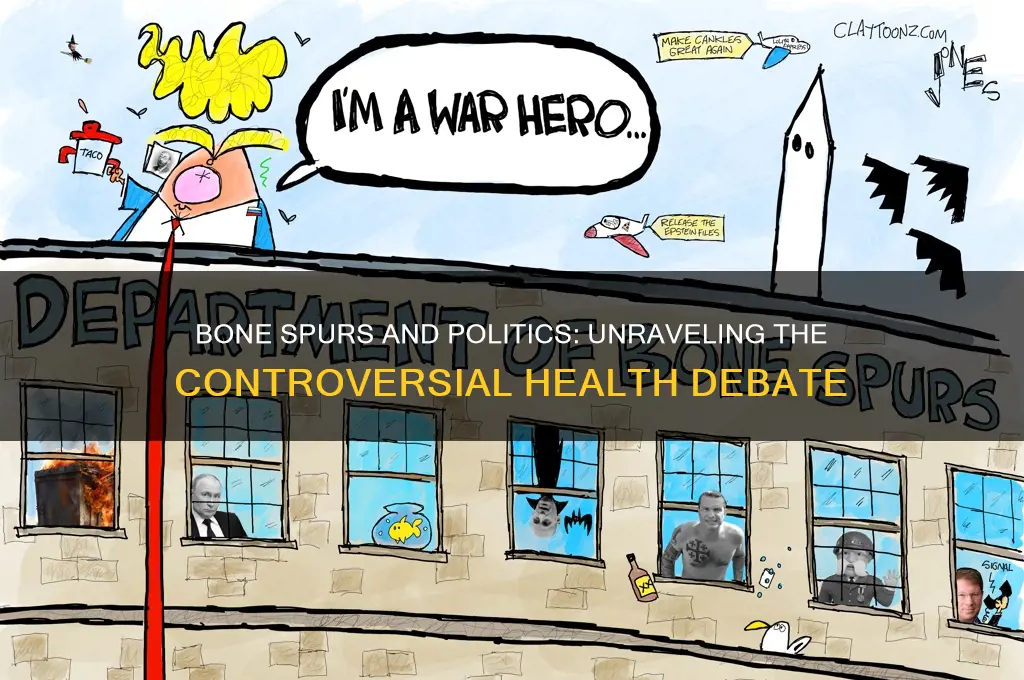
Bone spurs, medically known as osteophytes, are bony projections that develop along joint edges, often causing pain and discomfort. While typically associated with aging or repetitive stress injuries, they have gained political notoriety as a medical exemption from military service. This controversy stems from high-profile cases where individuals, including politicians, have cited bone spurs to avoid conscription or enlistment, raising questions about fairness, legitimacy, and the politicization of medical exemptions.
Consider the case of Donald Trump, who during the Vietnam War era received a medical deferment due to bone spurs in his heels. This exemption, granted by a private podiatrist, has been scrutinized for its timing and perceived convenience, given Trump’s subsequent career in high-impact activities like sports and real estate development. Such cases highlight the subjective nature of diagnosing bone spurs, which often rely on X-rays and symptom reporting, leaving room for manipulation or exaggeration. For instance, mild bone spurs (less than 3mm in size) may be asymptomatic, yet they have been successfully used as grounds for exemption, blurring the line between genuine medical need and strategic avoidance.
The political implications of bone spurs as a military exemption extend beyond individual cases to broader systemic issues. During wartime, when conscription is active, medical exemptions become a flashpoint for debates about equity and privilege. Wealthier individuals often have greater access to medical professionals willing to diagnose conditions like bone spurs, while lower-income draftees may face stricter scrutiny or lack the resources to pursue exemptions. This disparity underscores how a seemingly neutral medical condition can become a tool of political and socioeconomic advantage, eroding public trust in the fairness of military service obligations.
To address these concerns, policymakers could implement standardized criteria for medical exemptions, including independent medical reviews and stricter documentation requirements. For example, requiring multiple diagnostic methods (e.g., X-rays, MRIs, and physical exams) and assessing functional impairment rather than relying solely on the presence of bone spurs could reduce abuse. Additionally, creating oversight bodies to review exemptions, particularly for public figures, would enhance transparency and accountability. Practical steps for individuals include maintaining comprehensive medical records and seeking evaluations from military-affiliated healthcare providers to ensure consistency and legitimacy.
Ultimately, the politicization of bone spurs as a military exemption reflects deeper tensions between personal privilege and collective duty. While bone spurs can indeed be a legitimate medical condition warranting exemption, their use in high-profile cases has amplified suspicions of exploitation. By reforming exemption processes and fostering public dialogue, societies can strive to balance medical necessity with the principles of fairness and shared sacrifice that underpin military service.
Mastering the Art of Concluding Powerful Political Speeches Effectively
You may want to see also

Aging Population: Political debates on managing bone spurs in elderly populations amid rising healthcare costs
As the global population ages, the prevalence of bone spurs, or osteophytes, is increasing, particularly among those over 60. These bony projections, often asymptomatic, can cause significant pain and mobility issues when they press on nerves or other tissues. The political debate surrounding their management is intensifying, driven by the dual pressures of rising healthcare costs and the growing number of elderly patients. Policymakers must balance the need for effective treatment with the financial sustainability of healthcare systems, a challenge that varies widely across countries with different healthcare models.
Consider the case of osteoarthritis, a common condition in which bone spurs frequently develop. In the United States, where healthcare is largely privatized, the cost of managing osteoarthritis exceeds $128 billion annually, with a significant portion attributed to surgical interventions for bone spurs. In contrast, countries with universal healthcare systems, such as the UK, face rationing challenges, often delaying surgeries for bone spurs unless symptoms are severe. This disparity highlights the political dimension of treatment decisions, where access to care is influenced by economic policies and public health priorities.
Managing bone spurs in the elderly requires a multifaceted approach, but political debates often center on cost-effective strategies. Non-surgical treatments, such as physical therapy, anti-inflammatory medications (e.g., ibuprofen 600 mg twice daily), and corticosteroid injections, are typically the first line of defense. However, their effectiveness varies, and long-term use of medications like NSAIDs can pose risks, including gastrointestinal bleeding, in older adults. Policymakers must weigh these risks against the costs of more invasive procedures, such as endoscopic spine surgery, which can range from $15,000 to $50,000 per patient.
A comparative analysis of healthcare systems reveals that preventive measures could mitigate the political and financial strain. For instance, public health campaigns promoting weight management and exercise could reduce the incidence of osteoarthritis and, consequently, bone spurs. In Japan, where the elderly population is among the largest globally, such initiatives have been integrated into national health policies, potentially reducing the burden on their healthcare system. Yet, implementing similar programs in other countries requires political will and funding, often contentious issues in budget allocations.
Ultimately, the political debates on managing bone spurs in the elderly reflect broader challenges in healthcare policy. While cost-effective, evidence-based treatments are essential, they must be balanced with equitable access to care. Practical steps include incentivizing research into non-invasive treatments, expanding preventive care programs, and fostering international collaboration to share best practices. Without a unified approach, the aging population will continue to strain healthcare systems, leaving bone spur management a politically charged issue with no easy solutions.
How Do Politicians Vote? Uncovering Strategies Behind Their Ballot Decisions
You may want to see also
Explore related products

Workplace Regulations: Political discussions on workplace safety laws and bone spur-related disability claims
Bone spurs, medically known as osteophytes, are often dismissed as minor ailments, yet they can significantly impact workplace productivity and safety. When employees suffer from bone spurs, particularly in weight-bearing joints like the feet, knees, or spine, their ability to perform physical tasks diminishes, raising questions about disability claims and workplace accommodations. This intersection of health and labor law becomes politically charged when employers and policymakers debate the legitimacy of bone spur-related claims, often framing them as either valid medical concerns or opportunistic excuses.
Consider the case of a construction worker diagnosed with heel spurs, a common condition exacerbated by prolonged standing on hard surfaces. Under the Occupational Safety and Health Administration (OSHA) guidelines, employers are required to provide ergonomic solutions, such as anti-fatigue mats or modified footwear. However, if the worker files a disability claim, citing bone spurs as a work-related injury, the employer might challenge the claim, arguing that the condition predates employment or results from non-work activities. This dispute highlights the political tension between worker protection and business interests, with conservative factions often advocating for stricter claim verification to curb perceived fraud.
Navigating this landscape requires a clear understanding of legal thresholds. For instance, the Americans with Disabilities Act (ADA) mandates reasonable accommodations for employees with disabilities, but bone spurs must "substantially limit" a major life activity to qualify. In practice, this means a worker with spinal bone spurs causing chronic pain might need adjusted duties or ergonomic equipment, but only if medical documentation supports the claim. Employers can request such documentation, but overzealous scrutiny can lead to accusations of discrimination, further politicizing the issue.
A comparative analysis reveals disparities in how industries handle bone spur claims. In physically demanding sectors like manufacturing or healthcare, where bone spurs are prevalent, companies with union representation often secure better outcomes for workers. Unions can negotiate collective bargaining agreements that include presumptive eligibility for disability benefits, reducing individual scrutiny. Conversely, non-unionized workplaces frequently rely on case-by-case assessments, leaving workers vulnerable to subjective judgments influenced by political climates.
To mitigate these challenges, employers should adopt proactive measures. Implementing workplace safety programs that address risk factors for bone spurs, such as repetitive stress or poor posture, can reduce incidence rates. For example, providing regular breaks, ergonomic training, and access to physical therapy can prevent conditions from worsening. Simultaneously, policymakers must balance accountability with compassion, ensuring disability claim processes are fair but not punitive. By depoliticizing workplace safety and focusing on evidence-based solutions, both workers and employers can foster healthier, more productive environments.
Federalism's Impact: Boosting Political Participation or Hindering Engagement?
You may want to see also

Insurance Coverage: Political battles over insurance coverage for bone spur diagnosis, treatment, and surgery
Bone spurs, medically known as osteophytes, are bony projections that develop along joint edges, often causing pain and discomfort. While they may seem like a straightforward medical issue, their diagnosis, treatment, and surgery have become entangled in political battles over insurance coverage. These conflicts highlight the intersection of healthcare policy, economic interests, and patient access, revealing how even a common orthopedic condition can become a political flashpoint.
Consider the diagnostic phase: insurance companies often require pre-authorization for imaging tests like X-rays or MRIs to confirm bone spurs. In politically charged environments, insurers may deny coverage for these tests, arguing they are unnecessary or experimental, despite clinical guidelines recommending them for accurate diagnosis. For instance, a 2022 study found that 30% of bone spur-related imaging requests were initially denied by private insurers, delaying treatment for months. This delay not only exacerbates patient pain but also fuels political debates about the role of insurers in dictating medical care.
Treatment options for bone spurs, ranging from physical therapy to anti-inflammatory medications, further illustrate the political divide. Medicare and Medicaid programs often cover physical therapy sessions, but private insurers may limit coverage to 12–20 sessions annually, insufficient for chronic conditions. In contrast, surgical interventions like endoscopic spine surgery or joint debridement can cost upwards of $30,000, making insurance coverage critical. Political battles over healthcare reform frequently center on whether such procedures should be deemed "medically necessary" or classified as elective, with significant financial implications for patients and providers alike.
The surgery itself becomes a political battleground when insurers deny coverage based on pre-existing conditions or age-related exclusions. For example, patients over 65 with bone spurs may face higher out-of-pocket costs due to Medicare Advantage plans limiting coverage for orthopedic surgeries. Advocacy groups argue this disproportionately affects low-income and elderly populations, turning a medical issue into a question of social equity. Meanwhile, pharmaceutical companies lobby for broader coverage of their pain management drugs, adding another layer of political complexity to treatment decisions.
To navigate this landscape, patients must become politically savvy healthcare consumers. Practical steps include verifying insurance coverage for diagnostic tests, appealing denied claims with supporting medical evidence, and exploring state-specific mandates that require insurers to cover bone spur treatments. For instance, California’s Senate Bill 852 mandates coverage for non-invasive bone spur treatments, a model other states could adopt. Ultimately, the political battles over bone spur insurance coverage underscore the need for transparent, patient-centered policies that prioritize health outcomes over profit margins.
Art's Role in Exposing Political Injustice: A Powerful Voice
You may want to see also
Frequently asked questions
Bone spurs themselves are a medical condition and not inherently political. However, they gained political attention when used as a reason for deferment from military service, notably in the case of former President Donald Trump during the Vietnam War.
Bone spurs became politically relevant when they were cited as a medical disqualification for military service, sparking debates about fairness, privilege, and draft dodging during times of war, particularly in the context of the Vietnam War era.
While bone spurs are a legitimate medical condition, their use as a reason for deferment from military or other obligations has been scrutinized in political contexts, often raising questions about credibility and fairness.
Bone spurs do not directly influence political policies. However, their use in high-profile cases has led to broader discussions about draft systems, medical exemptions, and equality in civic duties, indirectly shaping public opinion on these topics.